Understanding Trt Duration: Detection Times, Dosage, And Metabolism
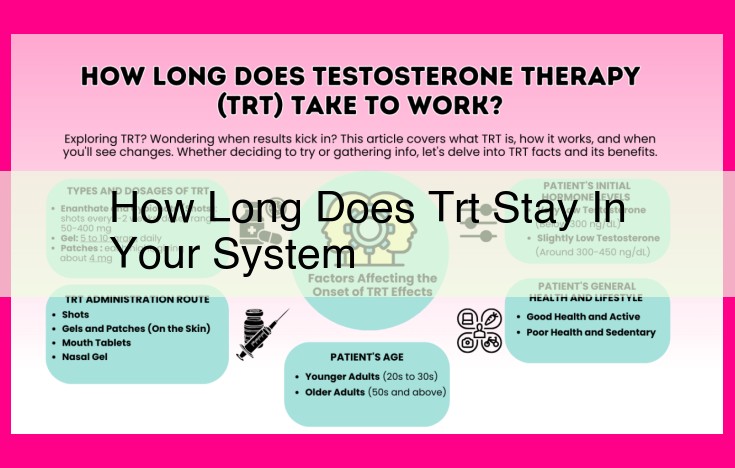
The duration of TRT in the system depends on the type of administration, dosage, and individual metabolism. Injections can remain detectable for several weeks or even months, while patches and gels may be cleared faster. Medical professionals involved in TRT, including endocrinologists and urologists, use blood tests and testosterone levels to determine the appropriate dosage and monitor the effects of therapy.
Endocrinologists: Specialists who diagnose and treat hormonal imbalances, including testosterone levels.
Endocrinologists: Guardians of Hormonal Balance
In the realm of testosterone therapy, endocrinologists stand as the gatekeepers of hormonal harmony, expertly diagnosing and treating imbalances, including testosterone levels. These medical wizards possess an unparalleled understanding of the delicate interplay of hormones within the human body.
As the architects of hormonal equilibrium, endocrinologists meticulously analyze blood samples, deciphering the intricate dance of testosterone levels. Armed with this knowledge, they skillfully determine the need for testosterone therapy, ensuring that each patient receives the precise dosage required to restore their hormonal symphony.
With their specialized expertise, endocrinologists guide patients through the complexities of testosterone therapy, addressing any concerns and monitoring progress with unwavering vigilance. They serve as compassionate companions on the path to hormonal restoration, dedicated to improving the lives of those who seek their guidance.
Urologists: Experts in Testosterone Therapy and Male Reproductive Health
When it comes to testosterone therapy, urologists play a pivotal role as highly specialized surgeons who focus on the urinary tract and male reproductive system. These skilled professionals wield a deep understanding of testosterone’s intricate influence on male health and are equipped with the expertise to provide comprehensive care.
Urologists possess a unique blend of medical and surgical knowledge, enabling them to diagnose and treat a wide range of conditions related to testosterone levels. They are trained to assess testosterone levels through blood tests and determine whether testosterone replacement therapy is necessary to address hormonal imbalances.
In cases where testosterone therapy is deemed appropriate, urologists offer a range of treatment options. Testosterone injections are a common method of administration, providing a convenient and effective way to replenish testosterone levels. Urologists are also proficient in administering testosterone patches, which release testosterone through the skin. These patches provide a more controlled and extended release, making them a suitable choice for certain individuals.
Beyond hormone replacement therapy, urologists also specialize in surgical procedures related to the male reproductive system. For transgender individuals seeking gender-affirming care, urologists play a critical role in performing surgeries to align the external genitalia with their gender identity. These complex and sensitive procedures require the delicate touch and expertise of a skilled urologist.
In addition to providing medical and surgical interventions, urologists serve as valuable educators and resources for individuals seeking information about testosterone therapy. They can provide comprehensive explanations about the potential benefits and risks associated with treatment and guide patients through the decision-making process.
If you are considering testosterone therapy, consulting with a qualified urologist is essential. These highly trained specialists possess the knowledge, experience, and surgical skills to ensure safe and effective treatment tailored to your specific needs. By partnering with a urologist, you can embark on a personalized journey towards optimal testosterone levels and enhanced overall well-being.
The Vital Blood Test: Unlocking the Secrets of Testosterone Levels
When it comes to testosterone therapy, the first step towards a tailored treatment plan is a comprehensive blood test. This essential assessment grants healthcare professionals a window into your testosterone levels, illuminating whether this hormone replacement therapy is the right path for you.
Picture this: a small sample of your precious blood embarks on a diagnostic journey. It whispers its secrets to a laboratory, where it undergoes a meticulous analysis. The result? A precise measurement of your testosterone concentration, a crucial piece of the puzzle in determining the necessity of testosterone therapy.
Beyond its binary verdict, this blood test provides invaluable insights into your hormonal landscape. It unveils not only the total testosterone circulating through your veins but also its unbound or “free” component. This distinction is paramount, as free testosterone is readily available to exert its biological effects in your body.
The significance of this blood test cannot be overstated. It serves as the cornerstone upon which an individualized testosterone therapy plan is built. By meticulously evaluating your testosterone levels, healthcare professionals can determine the optimal dosage and administration method that will restore your hormonal balance and empower you to regain your vitality.
Testosterone Injections: A common method of administering testosterone replacement therapy.
Testosterone Injections: The Cornerstone of Testosterone Replacement Therapy
Testosterone therapy is a vital medical intervention for individuals with low testosterone levels, often referred to as hypogonadism. Testosterone injections, the most prevalent form of testosterone delivery, offer a safe and effective method to restore testosterone levels and alleviate the symptoms of hypogonadism.
Testosterone injections are typically administered once or twice weekly in the upper thigh, hip, or buttock. The injection site is rotated to prevent irritation. The injection process is relatively painless, involving the subcutaneous injection of a tiny needle into the fatty tissue beneath the skin.
The injected testosterone is released slowly into the bloodstream, providing a steady supply of the hormone over several days. This sustained release helps maintain optimal testosterone levels, reducing the need for frequent injections.
Testosterone injections have been shown to significantly improve the symptoms of hypogonadism, including:
- Increased muscle mass and strength
- Improved libido and sexual function
- Reduced body fat
- Enhanced mood and energy levels
Testosterone injections are generally considered safe when administered under medical supervision. However, it’s essential to follow the prescribed dosage and schedule, as excessive testosterone can lead to side effects such as acne, hair loss, and aggressive behavior.
Before initiating testosterone therapy, it’s crucial to consult with a medical professional to determine if it’s right for you. A thorough medical history and physical examination are essential to rule out any underlying medical conditions that may be causing low testosterone levels and to ensure that testosterone therapy is the best course of treatment.
Testosterone Patches: A Convenient and Effective Option for Testosterone Therapy
For individuals seeking testosterone replacement therapy, testosterone patches offer a convenient and effective alternative to injections. Unlike injections that require regular visits to a healthcare professional, these patches can be applied directly to the skin, providing a steady release of testosterone throughout the day.
The patches are designed with a unique adhesive that adheres securely to the skin while allowing the gradual absorption of testosterone. This steady release mimics the natural production of testosterone in the body, ensuring optimal therapeutic effects without the fluctuations associated with injections.
Applying testosterone patches is a simple and painless process. The patches are typically worn on the back, buttocks, or thigh, where they remain invisible under clothing. Patients can enjoy the freedom of self-administration, allowing them to manage their therapy discreetly and conveniently.
The patches are also an ideal option for individuals who experience anxiety or discomfort with injections. The painless application and steady release of testosterone can significantly reduce any apprehension associated with traditional treatment methods.
Overall, testosterone patches offer a convenient, effective, and less invasive approach to testosterone therapy. They provide a consistent and reliable source of testosterone, empowering patients to manage their condition discreetly and comfortably.
Testosterone Therapy: A Comprehensive Guide
Understanding Testosterone Therapy
Testosterone, a hormone produced by the testes, plays a vital role in various physiological processes, including muscle mass, strength, and sexual function. When testosterone levels decline with age or due to underlying medical conditions, testosterone therapy may be considered.
Medical Professionals Involved in Testosterone Therapy
Endocrinologists and urologists are the primary medical professionals involved in testosterone therapy. Endocrinologists specialize in hormone imbalances, while urologists are experts in the male reproductive system. Together, they diagnose and manage testosterone levels to optimize patient outcomes.
Medical Tests and Procedures for Testosterone Therapy
A blood test is the standard method for measuring testosterone levels. Based on the results, testosterone therapy may be initiated. Common methods include testosterone injections, which provide a direct and effective way to raise testosterone levels.
Pharmaceuticals for Testosterone Therapy
Various pharmaceutical options are available for testosterone therapy, including testosterone patches. These transdermal patches deliver testosterone through the skin, providing a steady and sustained release.
Regulatory and Oversight Entities
The Food and Drug Administration (FDA) plays a crucial role in regulating testosterone therapy medications and devices. The FDA ensures the safety and effectiveness of testosterone products, providing guidelines for proper use and monitoring.
Research and Educational Resources
Numerous organizations and institutions, such as the National Institutes of Health (NIH) and the Mayo Clinic, conduct research on testosterone therapy and provide educational materials. These resources help patients and healthcare professionals stay informed about the latest advancements and evidence-based practices in testosterone therapy.
Impact on Specific Populations
Testosterone therapy has a significant impact on transgender individuals, who may use it as part of gender-affirming care. By raising testosterone levels, transgender individuals can align their physical appearance and hormone profile with their gender identity.
Testosterone Therapy: A Comprehensive Guide
Medical Professionals and Testosterone Therapy
When considering testosterone therapy, it’s crucial to consult qualified medical professionals. Endocrinologists specialize in diagnosing and treating hormone imbalances, including testosterone deficiency. Urologists, who focus on the urinary tract and male reproductive system, are also involved in testosterone therapy.
Diagnostics and Procedures
To determine the need for testosterone therapy, blood tests are performed to measure testosterone levels. Testosterone injections are a common method of delivery, offering precise control over testosterone levels.
Pharmacological Options
Besides injections, testosterone therapy can be administered through patches. These transdermal patches release testosterone directly into the skin.
Regulatory and Educational Resources
The Food and Drug Administration (FDA) ensures the safety and efficacy of testosterone therapy medications and devices. For research and educational materials, the National Institutes of Health (NIH) is an invaluable resource. They conduct studies on testosterone therapy and provide comprehensive information.
Impact on Specific Populations
Testosterone therapy plays a vital role in the healthcare of specific populations. For transgender individuals, it’s an essential component of gender-affirming care, helping them align their physical appearance with their gender identity.
Testosterone therapy is a complex treatment option that requires careful consideration and collaboration with medical professionals. By understanding the various aspects of testosterone therapy, including the medical specialists involved, diagnostic procedures, pharmaceutical options, regulatory oversight, and its impact on specific populations, individuals can make informed decisions about their healthcare.
The Comprehensive Guide to Testosterone Therapy
Testosterone therapy plays a vital role in addressing hormonal imbalances and improving the health and well-being of individuals with low testosterone levels. Understanding the medical professionals, tests and procedures, medications, and regulatory oversight involved is essential for anyone considering testosterone therapy.
Medical Professionals and Diagnostic Tests
Endocrinologists, specializing in hormonal imbalances, and urologists, focusing on the male reproductive system, are the primary medical professionals involved in testosterone therapy. Blood tests accurately assess testosterone levels, guiding treatment decisions.
Testosterone Administration Methods
Testosterone injections provide a direct and effective method of testosterone replacement. For those seeking a less invasive option, testosterone patches offer transdermal delivery through the skin.
Regulatory Oversight
The Food and Drug Administration (FDA) strictly regulates testosterone therapy medications and devices, ensuring patient safety and the efficacy of treatments.
Research and Education
The National Institutes of Health (NIH) conducts extensive research on testosterone therapy, providing valuable insights and educational materials. Renowned medical institutions like the Mayo Clinic offer comprehensive testosterone therapy services and research, providing evidence-based care for patients.
Impact on Transgender Individuals
For transgender individuals, testosterone therapy is a crucial component of gender-affirming care. It supports their physical, mental, and social transition toward their authentic gender identity.
Testosterone therapy is a highly personalized treatment that requires careful consideration and ongoing monitoring by qualified healthcare professionals. By understanding the medical aspects, regulatory oversight, and potential impact on specific populations, individuals can make informed decisions about testosterone therapy and optimize their health outcomes.
Testosterone Therapy: A Guide for Transgender Individuals
Testosterone therapy is an important part of gender-affirming care for transgender individuals. It can help to transform their physical appearance, improve their mood, and boost their self-esteem.
For transgender men, testosterone injections can help to build muscle mass, deepen the voice, and distribute body fat in a more masculine pattern. Testosterone patches can also be used, but they may be less effective than injections.
For transgender women, testosterone therapy can be used to help reduce body hair and muscle mass, and to increase breast size. It can also help to regulate menstrual cycles and affect fertility.
Before starting testosterone therapy, it’s important to talk to a healthcare provider to discuss the risks and benefits. Testosterone therapy can have a number of side effects, including acne, oily skin, hair loss, and changes in mood. It can also affect fertility.
If you’re considering testosterone therapy, it’s important to find a healthcare provider who is experienced in transgender care. They can help you to determine the best dosage and method of administration for your individual needs.
The Benefits of Testosterone Therapy for Transgender Individuals
Testosterone therapy can have a profound impact on the lives of transgender individuals. It can help them to:
- Feel more comfortable in their bodies
- Improve their mood and self-esteem
- Reduce body hair and muscle mass
- Increase breast size
- Regulate menstrual cycles
- Affect fertility
The Risks of Testosterone Therapy for Transgender Individuals
Testosterone therapy can also have a number of side effects, including:
- Acne
- Oily skin
- Hair loss
- Changes in mood
- Affect fertility
Finding a Healthcare Provider
If you’re considering testosterone therapy, it’s important to find a healthcare provider who is experienced in transgender care. They can help you to determine the best dosage and method of administration for your individual needs.