Testosterone’s Impact On Blood Donation: Trt Guidelines And Waiting Periods
Testosterone, a hormone produced naturally in the body, can affect blood donation guidelines. While testosterone is not typically a disqualifying factor, individuals on testosterone replacement therapy (TRT) may be subject to specific guidelines. Medical organizations recommend that individuals receiving TRT wait at least three months after their last injection before donating blood to ensure that their hemoglobin levels have returned to normal.
Medical Organizations Involved in Blood Donation
In the realm of healthcare, blood donation stands as a vital act of altruism, providing a lifeline to countless individuals in need. A network of medical organizations plays an indispensable role in this life-saving endeavor, each contributing their expertise to ensure the safety, efficiency, and accessibility of blood donations.
One prominent organization is the American Red Cross, renowned for its extensive blood collection and distribution services. Through its nationwide network of blood banks, the Red Cross caters to hospitals and medical facilities across the country, supplying essential blood products for emergencies, surgeries, and transfusions.
Joining the Red Cross in this vital mission is Blood Centers of America, a non-profit organization representing a network of community blood centers. These centers specialize in local collection and distribution of blood, ensuring a reliable supply to meet the needs of their respective regions.
Vitalant, another esteemed organization, operates as a not-for-profit blood bank serving hospitals and patients in multiple states. Its comprehensive services encompass blood collection, distribution, and testing, ensuring the highest standards of safety and quality for donated blood.
OneBlood stands out as a prominent blood bank in Florida, known for its innovative approach to blood donation. By implementing state-of-the-art technology and partnering with local organizations, OneBlood aims to enhance the donor experience and make blood donation more accessible to communities.
Government Agencies: Ensuring the Safety and Efficacy of Blood Donations
In the realm of blood donation, government agencies play a pivotal role, safeguarding the safety and efficacy of the process. Two prominent organizations, the Food and Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC), collaborate to ensure that donated blood meets the highest standards.
The FDA, as the federal regulatory agency, oversees the safety of blood and blood products. It establishes strict guidelines for blood collection, processing, and storage. These guidelines minimize the risk of contamination and transmission of infectious diseases. The FDA also inspects blood collection centers and manufacturers to ensure compliance with these regulations.
Complementing the FDA’s efforts, the CDC provides guidance and support for blood donation practices. Its role includes:
- Developing guidelines and recommendations: The CDC establishes guidelines for donor eligibility, blood screening, and transfusion practices to prevent the spread of disease and ensure patient safety.
- Monitoring bloodborne pathogens: The CDC tracks the prevalence and trends of bloodborne pathogens, such as HIV and hepatitis, to assess the effectiveness of screening methods and identify high-risk populations.
- Educating healthcare professionals and the public: The CDC provides educational materials and training programs to educate healthcare professionals and the general public about blood donation and transfusion safety.
The FDA and CDC work together tirelessly behind the scenes to ensure that every blood donation is safe and that every patient receives the necessary blood transfusions. Their unwavering commitment to regulation and monitoring safeguards the health and well-being of countless individuals.
Patient Advocacy Groups: Ensuring the Voices of Blood Donors and Recipients Are Heard
In the world of blood donation, the role of patient advocacy groups is paramount. These organizations serve as the cornerstone of representation, amplifying the needs and interests of those who generously give blood and those who rely on transfusions for their well-being.
Patient advocacy groups, with their passion and dedication, bridge the gap between individuals and healthcare systems. They offer invaluable support to blood donors by advocating for fair treatment, transparent information, and access to safe and reliable blood. Additionally, these groups provide a platform for blood recipients to share their experiences, raise awareness, and contribute to research and policy changes that improve transfusion practices.
One such group, the American Red Cross Blood Services Patient Advocacy Program, is dedicated to supporting patients throughout their blood donation and transfusion journey. Through its extensive network of volunteer advocates, the program provides emotional support, educational resources, and guidance to patients and their families. By empowering patients with knowledge and resources, they ensure that their voices are heard and their needs are prioritized.
Another notable organization, the National Marrow Donor Program (NMDP), plays a crucial role in advocating for patients with leukemia, lymphoma, and other blood-related disorders who require bone marrow or stem cell transplants. Through its tireless efforts, the NMDP has expanded the Registry’s diversity, increased donor access, and promoted research to improve transplant outcomes.
Patient advocacy groups are indispensable in the landscape of blood donation and transfusion medicine. Their unwavering commitment to patient well-being and unwavering advocacy for their needs serves as a catalyst for progress. By amplifying the voices of blood donors and recipients, they empower individuals, improve healthcare outcomes, and pave the way for a more equitable and compassionate blood donation system.
The Critical Need for Blood Donations: Saving Lives and Enhancing Health Outcomes
Blood donations are a vital component of our healthcare system, playing an indispensable role in saving lives and improving health outcomes. The demand for blood is constant, as it is used in various lifesaving procedures and treatments. This article delves into the critical need for blood donations and their profound impact on the well-being of our communities.
Saving Lives in Emergency Situations:
In emergency situations, such as accidents or disasters, blood transfusions can be the difference between life and death. Victims of severe injuries or burns may require immediate blood transfusions to stabilize their condition and prevent fatal consequences. Blood donations ensure that sufficient blood products are available to meet the urgent needs of these patients.
Treating Chronic Conditions and Diseases:
Blood transfusions are essential for individuals with chronic conditions and diseases that affect their blood production or function. Patients with sickle cell anemia, cancer, and hemophilia rely on regular blood transfusions to manage their symptoms and improve their quality of life. Blood donations provide a lifeline for these patients, enabling them to live healthier and more fulfilling lives.
Supporting Complex Medical Procedures:
Complex medical procedures, such as surgeries, organ transplants, and childbirth, often require blood transfusions to ensure adequate blood supply and prevent complications. Blood donations provide the necessary resources for surgeons and physicians to perform these lifesaving procedures with confidence.
Blood donations are essential for saving lives and improving health outcomes in our communities. By donating blood, we not only give a part of ourselves but also contribute to a precious and life-sustaining resource. Every unit of donated blood has the potential to transform the lives of multiple patients, giving them a second chance or a brighter future. It is a selfless act that makes a tangible difference in the well-being of our society.
Eligibility and Safety Considerations in Blood Donation
Blood donation is a noble act that saves countless lives. However, it’s crucial to ensure both the safety of the donor and the recipient. To maintain optimal safety standards, certain eligibility criteria and risk assessments are in place.
Donor Eligibility:
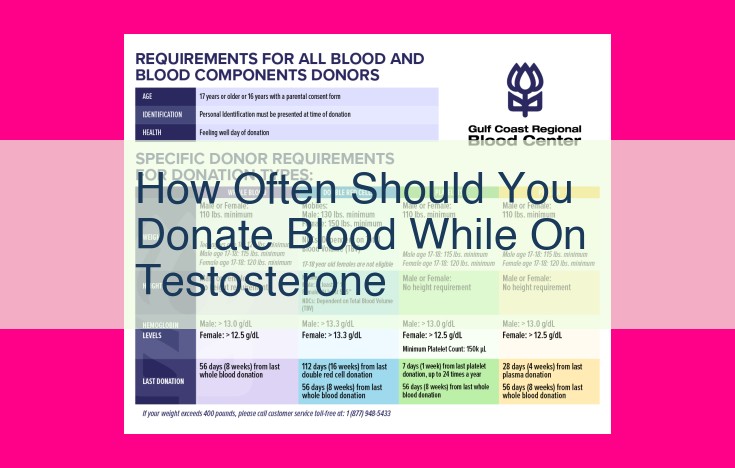
Who can donate blood? Generally, individuals between 17-75 years of age, weighing at least 110 pounds, and in good overall health are eligible. However, some factors may temporarily disqualify you, such as recent tattoos or piercings, travel to certain countries, or certain medications.
Potential Risks:
Blood donation is generally safe, but like any medical procedure, it carries minimal risks. These include temporary discomfort at the injection site, lightheadedness, or bruising. The most serious but rare risk is a vasovagal reaction, which can cause fainting.
Safety Measures:
To ensure maximum safety, all donated blood undergoes rigorous testing to screen for diseases like HIV, hepatitis, and syphilis. Additionally, blood collection centers follow strict hygiene protocols to minimize the risk of infection. Furthermore, autologous donations, where you donate blood for your own use, eliminate the risk of disease transmission.
Iron Levels:
Iron is essential for red blood cell production. To ensure donors have adequate iron levels, hemoglobin levels are checked prior to donation. Low hemoglobin can lead to anemia and potential health complications for both the donor and recipient.
Other Considerations:
Certain medical conditions, vaccinations, or recent pregnancies may affect eligibility to donate. If you have any concerns or questions, consult with a healthcare professional or contact your local blood donation center for guidance.
By adhering to eligibility criteria and safety protocols, we can ensure that blood donations are safe and beneficial for those who rely on them. If you are eligible, consider becoming a regular blood donor. Your altruistic act can save lives and make a profound difference in the health of our communities.
The Process of Blood Donation: A Step-by-Step Guide
Donating blood is a selfless act that can save lives. The process is relatively simple and takes about an hour. Here’s a step-by-step guide to help you prepare and understand what to expect:
Registration
When you arrive at the donation center, you’ll need to register. This involves providing your personal information, medical history, and answering a few questions about your current health.
Screening
Once you’re registered, you’ll be taken to a screening area. A staff member will take your temperature, pulse, and blood pressure. They’ll also ask you some additional questions about your health and travel history.
If you meet the eligibility requirements, you’ll be given a health questionnaire to complete. This questionnaire will ask you about any recent illnesses, medications you’re taking, and any other factors that could affect your ability to donate blood.
Collection
If you pass the screening, you’ll be taken to the donation area. You’ll be asked to sit in a comfortable chair and a staff member will insert a needle into a vein in your arm. The blood will flow through the needle into a sterile bag.
The entire process usually takes 8-10 minutes, but it can take longer if you have small veins or if you’re donating a large amount of blood.
Storage
Once the blood has been collected, it will be stored in a refrigerated facility. The blood will be tested to ensure that it is safe to transfuse.
Aftercare
After you donate blood, you’ll be given some snacks and juice to help you recover. You may experience some minor side effects, such as bruising, soreness, or lightheadedness. These side effects usually go away within a few hours.
Donating blood is a safe and rewarding experience. By donating, you can help save lives and improve the health of others.
Research and Innovation: Advancing Blood Transfusion Medicine
Blood transfusion medicine is continuously evolving, thanks to dedicated research and technological advancements. Scientists are exploring innovative solutions to enhance the safety, efficacy, and availability of blood transfusions.
One area of progress lies in the development of improved blood storage methods. Traditional blood storage techniques rely on refrigeration, which has limited preservation time. Recent breakthroughs, such as cryopreservation, allow blood products to be stored at ultra-low temperatures for extended periods, preserving their viability. This extended shelf life can facilitate blood availability in remote areas or during emergency situations.
Advancements in screening methodologies are also revolutionizing blood transfusion practices. Highly sensitive and precise tests are being developed to detect a wider range of infectious agents, including emerging pathogens. By improving the accuracy of blood screening, these tests reduce the risk of transfusion-transmitted infections and enhance patient safety.
Additionally, researchers are exploring the potential of artificial blood substitutes. These synthetic substances mimic the properties of red blood cells, offering a promising alternative for patients who are ineligible for traditional blood transfusions. Artificial blood substitutes can be universally compatible, reducing the need for blood typing and cross-matching, and they have a longer shelf life than whole blood.
Ongoing research in blood transfusion medicine paves the way for safer, more effective, and accessible blood products. These breakthroughs have the power to transform healthcare, improving patient outcomes and saving countless lives. By investing in innovation and research, we can ensure that the future of blood transfusions is brighter than ever.
Blood Transfusion and Medical Uses
Blood transfusions are a vital medical procedure that can save lives and improve health outcomes for countless individuals. These transfusions involve replacing lost or damaged blood with donated blood to restore the body’s ability to function properly.
Various medical conditions and procedures necessitate blood transfusions. One common reason is hemorrhage, or excessive bleeding, which can occur during surgeries, accidents, or childbirth. Blood transfusions can replenish the lost blood and stabilize the patient’s vital signs.
Blood transfusions are also crucial for treating anemia, a condition characterized by low red blood cell count. Anemic patients may experience fatigue, shortness of breath, and pale skin. Blood transfusions can increase their red blood cell count and alleviate these symptoms.
Additionally, blood transfusions play a vital role in the treatment of blood disorders, such as sickle cell disease and leukemia. These disorders interfere with the production and function of blood cells, and transfusions can provide the necessary healthy blood cells to maintain the body’s health.
During blood transfusions, different blood components may be used, depending on the patient’s needs. Whole blood contains all the components of blood, including red blood cells, white blood cells, platelets, and plasma. Red blood cell concentrate is used to treat anemia, while platelet concentrate is used to prevent or stop bleeding. Plasma is the liquid component of blood and is used to treat conditions such as shock and burns.
The importance of blood donation cannot be overstated, as it provides a critical resource for saving lives and improving health. By donating blood, individuals can make a significant contribution to the well-being of their community and those in need.