Understanding Semaglutide Dosing: Converting Units For Optimal Diabetes Management
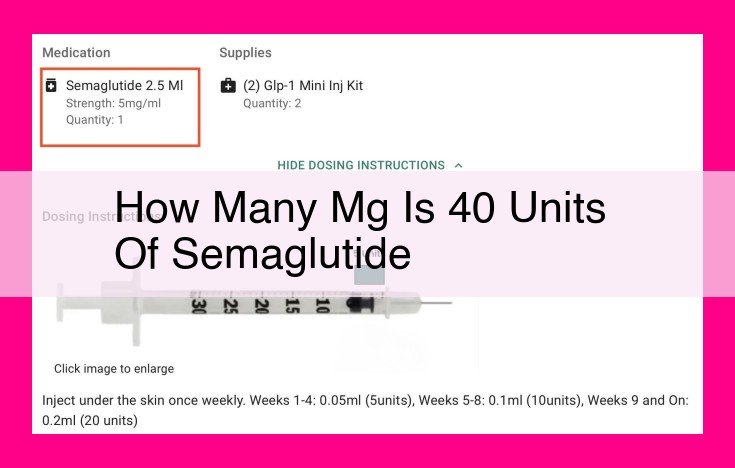
40 units of semaglutide is equivalent to 0.24 mg. Semaglutide, a GLP-1 agonist, is used to improve glycemic control in type 2 diabetes and reduce cardiovascular risk. Accurate dosing is crucial, as semaglutide is available in fixed doses of 0.5 mg, 1 mg, and 2 mg. Understanding the different units used for diabetes medications ensures precise administration and optimal management of blood sugar levels.
Unlocking the Arsenal: Medications in Diabetes Management
The world of diabetes management is a complex landscape, and medications play a crucial role in this battle against high blood sugar. From semaglutide to GLP-1 agonists and other anti-diabetic medications, each agent has its unique story to tell.
Semaglutide: The Rising Star
Semaglutide, a relatively newcomer in the diabetes armamentarium, has quickly gained prominence as a game-changer. This injectable medication mimics a natural hormone called GLP-1, which plays a vital role in regulating blood sugar levels. Semaglutide works by stimulating insulin secretion, promoting satiety (feeling full), and slowing down gastric emptying.
GLP-1 Agonists: Mimicking Nature’s Insulin Regulator
Glucagon-like peptide-1 (GLP-1) is a marvel of nature, responsible for enhancing insulin production and reducing glucagon release, the hormone that raises blood sugar. GLP-1 agonists, like semaglutide, harness the power of GLP-1, providing a similar effect of lowering blood sugar and improving overall glucose control. These medications are commonly used in type 2 diabetes, where the body’s own insulin production is impaired.
Anti-Diabetic Medications: A Diverse Array
The arsenal of anti-diabetic medications extends beyond semaglutide and GLP-1 agonists, encompassing a range of options. Some medications increase insulin sensitivity, while others work by inhibiting glucose absorption or blocking glucose production. These medications are tailored to the specific needs of each patient, considering factors such as age, health status, and individual treatment goals.
Measuring Diabetes Medications: Units, Dosing, and Conversion
When managing diabetes, accurately measuring your medications is crucial. Understanding the different units used in diabetes measurements, such as milligrams (mg) and units, ensures proper dosing and optimal treatment outcomes.
Milligrams (mg) measure the weight of a medication, while units measure its strength or potency. Different types of diabetes medications, such as insulin and GLP-1 agonists, may have different potencies and therefore require different units of measurement.
For instance, insulin is usually measured in units, while GLP-1 agonists are typically measured in milligrams (mg). It’s essential to consult your healthcare provider or refer to the medication label for the correct units to use.
Accurate dosing is vital in diabetes management. Taking too much or too little medication can interfere with blood sugar control. Therefore, it’s crucial to follow your doctor’s prescription and use the correct measuring device.
If you encounter different units when converting between medications or adjusting your dosage, you may need to convert the units. Conversion charts or online calculators can assist with this process, ensuring accuracy and preventing medication errors.
Remember, proper dosing and measurement of diabetes medications are fundamental to managing the condition effectively. By understanding the different units and their significance, you can confidently participate in your treatment plan and achieve optimal health outcomes.
Physiological Processes Affected by Diabetes
Diabetes is a chronic condition characterized by elevated blood sugar levels. This condition arises when the body produces insufficient insulin or does not use insulin effectively. Insulin is a hormone produced by the pancreas that helps glucose enter cells for energy. Without adequate insulin, glucose accumulates in the bloodstream, leading to a cascade of health complications.
Glucose Metabolism
Glucose metabolism refers to the series of biochemical reactions that convert glucose into energy. In a healthy body, insulin facilitates glucose uptake into cells, where it is oxidized to produce adenosine triphosphate (ATP) – the cell’s primary energy currency.
Blood Sugar Regulation
Blood sugar regulation involves maintaining blood glucose levels within a narrow range. This regulation is crucial for optimal organ and tissue function. In non-diabetic individuals, insulin and other hormonal signals work in concert to control glucose production and utilization. In contrast, individuals with diabetes experience impaired glucose regulation due to insulin deficiency or resistance.
How Medications Improve Physiological Processes
Diabetes medications aim to improve physiological processes affected by diabetes. By supplementing insulin or enhancing insulin sensitivity, these medications can effectively lower blood sugar levels.
Enhancing Insulin Production and Action
Certain medications, such as insulin injectables, mimic the effects of natural insulin. These medications can enhance insulin production or increase insulin sensitivity, facilitating glucose uptake by cells.
Inhibiting Glucose Production
Other medications, known as GLP-1 agonists, work by stimulating the release of glucagon-like peptide-1 (GLP-1), a hormone that slows down gastric emptying and inhibits glucose production by the liver.
Promoting Glucose Utilization
SGLT2 inhibitors are another class of diabetes medications that promote glucose excretion through the urine. This mechanism helps reduce blood glucose levels.
Devices for Diabetes Medication Administration: Navigating the Arsenal for Optimal Management
When it comes to diabetes management, devices play a crucial role in the accurate and efficient administration of medications. These devices range from traditional insulin syringes to advanced insulin pumps, each with its unique advantages and considerations.
Insulin Syringes:
Insulin syringes are the most basic device used for insulin injection. They come in various sizes, allowing for precise dosing as per your doctor’s prescription. The needle size can also be customized based on your skin thickness and comfort level. Insulin syringes offer simplicity and portability, making them suitable for those who prefer a straightforward approach.
Insulin Pens:
Insulin pens are pre-filled with insulin and come with a built-in needle. They are convenient and easy-to-use, featuring a dial that allows for accurate dosing. Insulin pens eliminate the need for mixing insulin and reduce the risk of needle-stick injuries. However, they are disposable, adding to the ongoing cost.
Insulin Pumps:
Insulin pumps are small, computerized devices that continuously deliver insulin throughout the day via a small cannula (tube) inserted under the skin. They offer precise and customized insulin delivery, allowing for better control of blood sugar levels. While insulin pumps provide flexibility and convenience, they require regular maintenance and can be more expensive than other devices.
Which Device is Right for You?
The choice of device depends on your individual needs, preferences, and medical history. If you prefer a simple and portable option, insulin syringes or pens may suffice. For those seeking precise and customized insulin delivery, an insulin pump might be a better choice. Your healthcare provider will guide you in selecting the device that best meets your requirements.
Proper Use and Maintenance:
Regardless of the device you choose, proper use and maintenance are essential for safe and effective medication administration. Always follow the manufacturer’s instructions and your doctor’s recommendations carefully. Regularly inspect your devices for damage or malfunctions and ensure they are cleaned and stored appropriately.
Devices for diabetes medication administration are indispensable tools in managing the condition effectively. Understanding the different types of devices, their advantages, and how to use them properly empowers you to make informed decisions about your diabetes care. By working with your healthcare provider, you can find the device that best suits your unique needs and optimize your diabetes management journey.
The Role of Research and Clinical Trials in Revolutionizing Diabetes Management
As the medical world continues to advance at an unprecedented pace, research and clinical trials play a pivotal role in shaping the landscape of diabetes management. These meticulous studies delve into the efficacy and safety of novel medications like semaglutide, unlocking new horizons in the fight against diabetes.
Clinical Trials: Unlocking the Power of Semaglutide
Through rigorous clinical trials, researchers have meticulously assessed the effectiveness of semaglutide, a groundbreaking treatment for diabetes. In landmark studies, patients who received semaglutide experienced significant improvements in blood sugar control, weight loss, and reduced risk of cardiovascular complications.
Results that Transform Lives
The results of these clinical trials are not merely statistics; they represent tangible benefits that translate into improved health outcomes for people living with diabetes. For instance, the SUSTAIN 6 trial demonstrated that semaglutide reduced the relative risk of major adverse cardiovascular events (MACE) by an impressive 26%. This groundbreaking finding highlights the potential of semaglutide to not only manage blood sugar but also protect against life-threatening heart and stroke events.
Implications for Clinical Practice
The findings of these clinical trials have profound implications for clinical practice. Healthcare providers are now equipped with scientifically validated evidence to optimize the care of their diabetes patients. By prescribing medications like semaglutide, which have been rigorously tested and proven effective, they can confidently empower their patients to achieve better health outcomes and enjoy a better quality of life.
Continued Research: Driving Innovation and Progress
As the field of diabetes management continues to evolve, research and clinical trials remain essential engines of progress. Ongoing studies are exploring the potential of semaglutide for treating other chronic conditions, such as obesity and non-alcoholic fatty liver disease. These investigations hold immense promise, offering hope for improved health outcomes for an even wider population.