Semaglutide Units: Understanding Dosages In Ozempic And Wegovy For Diabetes And Obesity
I. Overview and Background
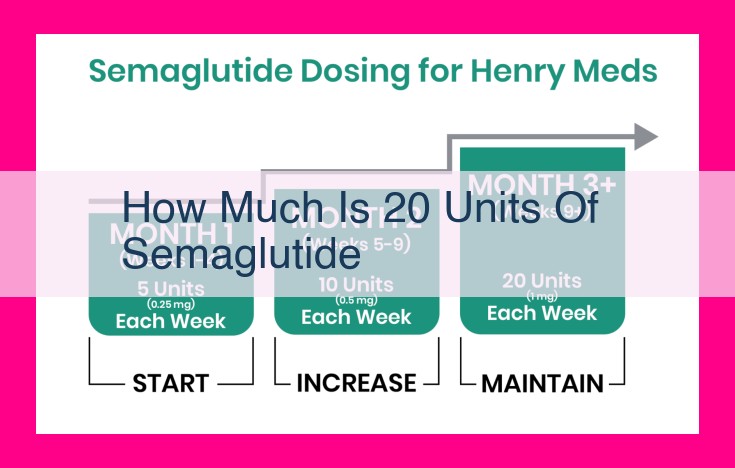
Semaglutide, a GLP-1 agonist used to treat type 2 diabetes and obesity, is typically administered in units. The amount of Semaglutide in 20 units depends on the specific formulation. For example, in the pen device (Ozempic), 20 units are equivalent to 1 mg of Semaglutide, while in the once-weekly injection (Wegovy), 20 units correspond to 2.4 mg.
Understanding the Epidemic of Type 2 Diabetes and Obesity
Type 2 diabetes is a chronic condition in which the body becomes resistant to insulin, a hormone that regulates blood sugar levels. Over time, this resistance can lead to persistently high blood sugar levels, increasing the risk of serious health complications like heart disease, stroke, kidney failure, and blindness.
Obesity is a condition characterized by an excessive amount of body fat. It is often measured by body mass index (BMI), a ratio of weight to height. Obesity is a significant risk factor for type 2 diabetes and other chronic diseases, such as heart disease, stroke, and some types of cancer.
Globally, the prevalence of type 2 diabetes and obesity has reached alarming levels. Approximately 463 million adults live with diabetes worldwide, and over 650 million adults are obese. These conditions are not just a concern for individuals but also a significant burden on healthcare systems worldwide.
The impact of type 2 diabetes and obesity on individuals and society is profound. For individuals, these conditions can lead to a diminished quality of life, reduced life expectancy, and increased healthcare costs. For society, the economic burden of these conditions is substantial, with the estimated global cost of diabetes alone reaching $1.3 trillion in 2021. Understanding the magnitude of the problem is crucial for developing effective strategies to address these prevalent health concerns.
Pharmaceutical Companies: Driving Innovation in GLP-1 Agonist Therapy
The pharmaceutical industry plays a crucial role in the development and marketing of GLP-1 agonists, a class of medications that have revolutionized the treatment of type 2 diabetes and obesity. These companies invest heavily in research and development, bringing innovative therapies to market that improve the lives of millions worldwide.
Among the key players in the GLP-1 agonist market are Novo Nordisk and Eli Lilly and Company. Novo Nordisk is a global healthcare company with a long history of innovation in diabetes care. They are the pioneers behind semaglutide, a highly effective GLP-1 agonist that has been approved for the treatment of both type 2 diabetes and obesity.
Eli Lilly and Company is another major player in the GLP-1 agonist market. They have developed dulaglutide, a long-acting GLP-1 agonist that is effective in controlling blood sugar levels and promoting weight loss. Both Novo Nordisk and Eli Lilly and Company have made significant contributions to the field of GLP-1 agonist therapy, helping to improve the lives of countless individuals with type 2 diabetes and obesity.
Medications for Type 2 Diabetes and Obesity: GLP-1 Agonists
GLP-1 agonists are a class of medications revolutionizing the treatment of type 2 diabetes and obesity. These groundbreaking drugs mimic the actions of a naturally occurring hormone called glucagon-like peptide-1 (GLP-1) in the body.
Mechanism of Action
GLP-1 agonists work by slowing down digestion, increasing insulin production, and suppressing appetite. This combination of effects reduces blood sugar levels, promotes weight loss, and improves insulin sensitivity.
Specific Medications
Some of the most well-known GLP-1 agonists include:
- Semaglutide (Ozempic, Wegovy): Long-acting injectable medication that has shown remarkable efficacy in lowering A1C levels and promoting weight loss.
- Liraglutide (Victoza): Once-daily injectable that has been approved for både diabetes and obesity management_.
- Dulaglutide (Trulicity): Weekly injectable that offers consistent blood sugar control and sustained weight loss.
Efficacy
Clinical studies have consistently shown that GLP-1 agonists are highly effective in:
- Lowering blood sugar levels in type 2 diabetes patients
- Promoting significant weight loss in obese individuals
- Improving insulin sensitivity
- Reducing the risk of cardiovascular events
GLP-1 agonists are a powerful tool in the fight against type 2 diabetes and obesity. By mimicking the body’s natural hormone, these medications effectively control blood sugar, promote weight loss, and improve overall health. As research continues, we can expect even more innovative and effective GLP-1 agonists to emerge in the future.
The Financial Burden of GLP-1 Agonists: A Deeper Look
Understanding the financial implications of GLP-1 agonists for type 2 diabetes and obesity is crucial for stakeholders involved in their development, prescription, and use. These medications have a significant impact on individuals and healthcare systems alike.
Wholesale Cost and Retail Price
The wholesale cost of GLP-1 agonists varies widely depending on the specific medication and dosage prescribed. For example, Semaglutide (brand name Ozempic) can range from $1,000 to $1,500 per month, while Liraglutide (brand name Saxenda) may cost around $1,200 to $1,800 per month.
The retail price, which is the cost to patients, may be even higher. This is especially true for those without insurance coverage or with high deductibles. In some cases, the retail price of a GLP-1 agonist can be several thousand dollars per month.
Insurance Coverage
Insurance coverage for GLP-1 agonists also varies widely. Some insurance plans may require patients to try cheaper medications first before approving coverage for GLP-1 agonists. Others may only cover GLP-1 agonists for patients with specific medical conditions or who have failed other treatments.
Affordability and Accessibility
The high cost of GLP-1 agonists can make them difficult for many patients to afford. This is especially true for those who are uninsured or underinsured. The lack of affordable access to GLP-1 agonists can lead to patients delaying or skipping treatment, which can have serious consequences for their health.
The financial implications of GLP-1 agonists is a complex issue that affects both patients and healthcare systems. The high cost of these medications can make them difficult for many patients to afford, while the lack of insurance coverage can further exacerbate this issue. It is important for stakeholders to work together to find ways to improve the affordability and accessibility of GLP-1 agonists so that all patients who need them can benefit from their life-changing effects.
Healthcare Providers and Patients: Perspectives and Experiences
Providers’ Perspectives
Healthcare providers play a critical role in the management of type 2 diabetes and obesity. They are the ones who prescribe GLP-1 agonists and monitor their patients’ progress. Providers have generally reported positive experiences with GLP-1 agonists. They have found that these medications are effective in lowering blood sugar levels and promoting weight loss. They have also noted that GLP-1 agonists are well-tolerated by most patients. Some providers have expressed concern about the cost of GLP-1 agonists, but they believe that these medications are worth the investment for patients who can benefit from them.
Patients’ Experiences
Patients who have used GLP-1 agonists have reported positive outcomes. They have found that these medications have helped them to control their blood sugar levels, lose weight, and improve their overall health. Patients have also reported that GLP-1 agonists have improved their quality of life. They have more energy, feel better about themselves, and are more active.
Side effects from GLP-1 agonists are generally mild and temporary. The most common side effects include nausea, vomiting, diarrhea, and constipation. These side effects usually go away after a few days or weeks.
Overall, patients have been very satisfied with GLP-1 agonists. They have found that these medications have helped them to manage their type 2 diabetes or obesity and improve their quality of life.
Challenges and Opportunities in the GLP-1 Agonist Market
Challenges:
Although GLP-1 agonists have revolutionized the management of type 2 diabetes and obesity, they face several challenges. One major barrier is limited insurance coverage. Many insurance plans either don’t cover GLP-1 agonists or impose strict restrictions and high co-pays, making them financially inaccessible for many patients.
Another challenge is the high cost of these medications. GLP-1 agonists are typically expensive, with some brands costing thousands of dollars per month. This poses a significant financial burden on patients, especially those who require long-term treatment.
Lastly, patient adherence can be an issue. GLP-1 agonists are typically injectable medications, which can be a barrier for some patients. Additionally, the effectiveness of these medications depends on consistent use, and forgetting or skipping doses can compromise their efficacy.
Opportunities:
Despite these challenges, there are opportunities to improve the accessibility and effectiveness of GLP-1 agonists. Innovation in drug development can lead to the creation of new GLP-1 agonists that are more affordable, easier to administer, and have fewer side effects.
Research is also crucial to enhance our understanding of the long-term effects and potential of GLP-1 agonists. Ongoing studies can provide insights into the role of these medications in preventing cardiovascular disease and other complications associated with type 2 diabetes and obesity.
Access improvement is paramount to ensure that all patients who can benefit from GLP-1 agonists have the opportunity to do so. This involves working with insurance companies to expand coverage, negotiating lower prices with manufacturers, and implementing financial assistance programs for low-income patients.
GLP-1 agonists have transformed the management of type 2 diabetes and obesity, but they also face challenges that limit their widespread use. By addressing these obstacles and embracing opportunities for innovation, research, and access improvement, we can empower more patients to live healthier, fuller lives.