Safeguard Against Excessive Bleeding: Discontinuing Blood Thinners For Tooth Extraction
How Long Should You Stop Blood Thinners Before Tooth Extraction?
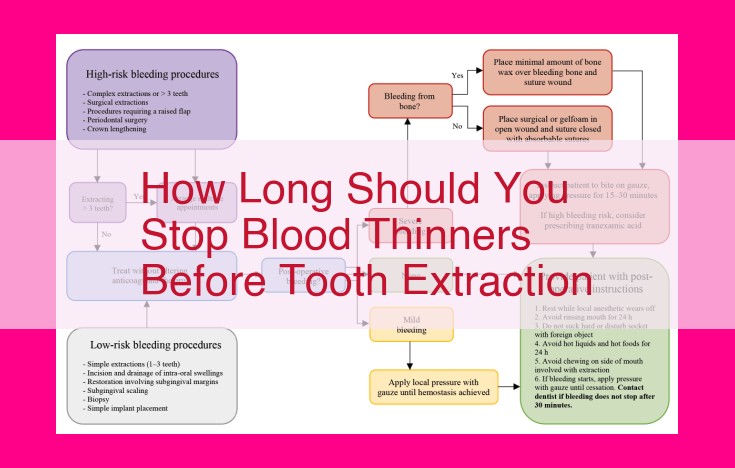
Before undergoing tooth extraction, it is crucial to discontinue blood thinners to minimize the risk of excessive bleeding. The duration of discontinuation depends on the type of blood thinner and the individual’s clotting profile. Typically, warfarin should be stopped 3-5 days before the procedure, while heparin can be stopped 24 hours prior. However, it is essential to consult with the healthcare provider to determine the appropriate time frame and any necessary adjustments to medication regimen, including aspirin or other anticoagulants.
**Navigating the Maze of Blood Clot-Related Medical Conditions**
Introduction:
Blood clots, a serious health concern, can strike without warning and have potentially life-threatening consequences. Understanding the medical conditions that increase your risk of developing blood clots is crucial for proactive prevention and timely treatment. This blog post will explore the complexities of deep vein thrombosis (DVT), pulmonary embolism (PE), atrial fibrillation (AFib), valvular heart disease, and congestive heart failure (CHF), equipping you with essential knowledge to protect your well-being.
1. Deep Vein Thrombosis (DVT)
DVT occurs when a blood clot forms in a deep vein, usually in the legs. Symptoms may include swelling, pain, warmth, and redness. Risk factors include prolonged inactivity, surgery, and certain medical conditions. If left untreated, DVT can lead to serious complications such as pulmonary embolism.
2. Pulmonary Embolism (PE)
PE is a life-threatening condition that occurs when a blood clot from a deep vein travels to the lungs, blocking blood flow. Symptoms may include sudden shortness of breath, chest pain, and rapid heart rate. Prompt medical attention is essential to dissolve the clot and prevent further complications.
3. Atrial Fibrillation (AFib)
AFib is an irregular and often rapid heart rhythm. It can increase the risk of stroke and blood clots. Symptoms may include palpitations, shortness of breath, and fatigue. Medications or procedures may be recommended to regulate the heart rhythm and reduce the risk of clots.
4. Valvular Heart Disease
Valvular heart disease occurs when the heart valves become damaged or malfunction. This can lead to blood clots forming in the heart chambers or near the valves. Symptoms vary depending on the severity and location of the valve damage. Treatment may involve medications, surgery, or a combination of both.
5. Congestive Heart Failure (CHF)
CHF is a condition in which the heart is unable to pump blood effectively. This can lead to fluid buildup in the body, including in the lungs, which can increase the risk of blood clots. Symptoms may include shortness of breath, fatigue, and swelling in the legs. Medications and lifestyle changes are typically recommended to manage CHF and reduce the risk of clots.
Understanding Medical Conditions Related to Blood Clots
Deep Vein Thrombosis (DVT)
DVT is a condition in which a blood clot forms in a deep vein, typically in the leg or pelvis. Symptoms may include leg or ankle pain, swelling, warmth, and redness. Risk factors include prolonged immobilization, obesity, age, smoking, and certain medical conditions like pregnancy and cancer. If left untreated, a DVT can travel through the body and cause a life-threatening pulmonary embolism (PE).
Pulmonary Embolism (PE)
A PE occurs when a blood clot lodges in one of the arteries supplying blood to the lungs. Symptoms may include sudden chest pain, shortness of breath, rapid heart rate, and coughing up blood. Risk factors are similar to those for DVT, and it’s a serious medical emergency requiring immediate treatment.
Atrial Fibrillation (AFib)
AFib is a heart rhythm disorder in which the upper chambers of the heart (atria) beat irregularly. This can increase the risk of blood clots forming in the atria and traveling to the brain, causing a stroke. Symptoms may include rapid heart rate, palpitations, shortness of breath, and fatigue. Risk factors include age, high blood pressure, obesity, and heart disease.
Valvular Heart Disease
Valvular heart disease occurs when the heart valves don’t function properly. This can lead to blood flow disturbances that increase the risk of blood clots forming in the heart or blood vessels. Symptoms may vary depending on the affected valve, but can include shortness of breath, fatigue, chest pain, and arrhythmias.
Congestive Heart Failure (CHF)
CHF is a condition in which the heart is unable to pump blood effectively, causing a buildup of fluid in the body. This can lead to reduced blood flow and an increased risk of blood clots forming in the heart or blood vessels. Symptoms may include shortness of breath, fatigue, swelling in the legs or ankles, and difficulty sleeping.
**Understanding the Role of Blood Thinners in Preventing Clots: A Patient-Friendly Guide**
Blood clots, also known as thrombosis, can be a serious health concern. If not treated promptly, they can lead to life-threatening complications such as pulmonary embolism (PE) or stroke. Fortunately, there are medications called blood thinners that can effectively prevent and treat blood clots.
One of the most commonly used blood thinners is warfarin, also known by its brand name Coumadin. It is an oral medication that has been used for decades to reduce the risk of clots in people with conditions like atrial fibrillation (AFib), valvular heart disease, and deep vein thrombosis (DVT).
Warfarin works by interfering with the body’s natural clotting process. It blocks the action of vitamin K, which is essential for the production of clotting factors. By reducing the levels of these factors, warfarin makes it less likely for clots to form.
Another commonly used blood thinner is heparin. Unlike warfarin, which is taken orally, heparin is administered intravenously or subcutaneously (under the skin). It works rapidly to prevent the formation of new clots and is often used in emergency situations or as a bridge therapy until warfarin can take effect.
Both warfarin and heparin have their own advantages and disadvantages. Warfarin is less expensive and can be taken at home, but it requires regular blood monitoring to ensure the dosage is correct. Heparin, on the other hand, does not require blood monitoring but may cause more side effects, such as bleeding and bruising.
Choosing the right blood thinner for you depends on your individual needs and risk factors. Your doctor will work with you to determine the best treatment plan and provide guidance on lifestyle adjustments and precautions to minimize the risks associated with blood thinners.
Understanding the Mechanism of Blood Thinners
Blood clots are a serious medical concern that can lead to life-threatening conditions such as deep vein thrombosis (DVT), pulmonary embolism (PE), and stroke. Blood thinners play a vital role in preventing and treating these clots, offering a lifeline to millions worldwide.
In this section, we delve into the mechanism of action of blood thinners, explaining how they work to keep your blood flowing freely and protect you from the dangers of clotting.
Unraveling the Clot Formation Process
To understand how blood thinners work, we must first grasp the process of blood clot formation. When blood vessels are injured, proteins in the blood, called coagulation factors, initiate a cascade of reactions that lead to the formation of a blood clot. This clot acts as a protective barrier, preventing excessive bleeding.
The Role of Blood Thinners
Blood thinners, often referred to as anticoagulants, work by interrupting the coagulation cascade at various points. They prevent or slow down the formation of blood clots without impairing normal blood flow.
Types of Blood Thinners and Their Mechanisms
Different types of blood thinners work in different ways to prevent clots.
-
Warfarin (Coumadin): This oral medication blocks the action of vitamin K, an essential nutrient for the production of certain coagulation factors. By reducing the levels of these factors, warfarin inhibits blood clot formation.
-
Heparin: A naturally occurring substance, heparin binds to a protein called antithrombin III. This complex then neutralizes other coagulation factors, effectively preventing clot formation. Heparin is often administered intravenously or subcutaneously.
-
Direct Oral Anticoagulants (DOACs): These newer oral medications target specific coagulation factors directly, inhibiting their activity. DOACs include drugs like apixaban (Eliquis), rivaroxaban (Xarelto), and edoxaban (Lixiana).
Monitoring and Management
To ensure optimal efficacy and minimize the risk of bleeding, regular blood monitoring is crucial when taking blood thinners. Your doctor will adjust your dosage based on the results of these tests.
It is also important to make lifestyle adjustments while taking blood thinners. Avoiding certain medications, foods, and activities that may interfere with their effectiveness or increase the risk of bleeding is essential. Your healthcare provider will provide specific guidance tailored to your individual needs.
By understanding the mechanism of blood thinners and working closely with your doctor, you can effectively manage your clotting risk and live a healthier, more fulfilling life.
Medical Conditions Related to Blood Clots
Blood clots, often referred to as thrombi, are a serious health concern that can lead to potentially life-threatening conditions like deep vein thrombosis (DVT) and pulmonary embolism (PE). Other medical conditions that increase the risk of blood clots include atrial fibrillation (AFib), valvular heart disease, and congestive heart failure (CHF).
Understanding the Symptoms and Risks
Recognizing the symptoms of blood clots is crucial. Deep vein thrombosis (DVT) typically manifests as swelling, pain, and tenderness in the affected leg. Pulmonary embolism (PE) occurs when a blood clot travels to the lungs and can cause sudden shortness of breath, chest pain, and coughing. Atrial fibrillation (AFib) is an irregular heartbeat that can lead to blood clots in the heart, while valvular heart disease and congestive heart failure can impair blood flow and increase the risk of clot formation.
Blood Thinners: Types and Mechanism of Action
Blood thinners, also known as anticoagulants, are medications used to reduce the risk of blood clots. Warfarin (Coumadin) and heparin are two commonly used blood thinners. Warfarin works by interfering with the body’s clotting process, while heparin prevents the formation of new clots.
Differences in Administration, Monitoring, and Side Effects
The administration and monitoring of warfarin and heparin differ significantly. Warfarin is taken orally, while heparin is administered intravenously or subcutaneously. Warfarin requires regular blood monitoring to ensure the dose is adjusted appropriately, whereas heparin does not.
Both warfarin and heparin can have side effects. Warfarin can increase the risk of bleeding, especially if the dose is too high. Heparin can cause bleeding, as well as an allergic reaction known as heparin-induced thrombocytopenia (HIT).
Recommendations for Prevention and Treatment
Preventing blood clots is essential. Regular exercise, maintaining a healthy weight, and avoiding prolonged inactivity can all help. Medications, such as blood thinners, may be prescribed for individuals with an increased risk of clotting due to underlying conditions.
If you experience any symptoms of a blood clot, such as sudden shortness of breath, chest pain, or swelling in your leg, seek medical attention immediately. Prompt diagnosis and treatment can significantly improve outcomes.
Blood Clots: Understanding the Elevated Risk with Age
Aging is an inevitable part of life, and with the passage of time comes an increased risk of various health ailments. Among these is the formation of blood clots, a condition that can have serious consequences. Understanding the connection between age and blood clots is crucial for maintaining good health and well-being.
As we grow older, our bodies undergo several physical changes that can make us more susceptible to developing blood clots. Our blood becomes thicker and more prone to clotting, and the walls of our blood vessels become less elastic. This combination of factors can create an environment where blood flow is compromised and clots are more likely to form.
The risk of blood clots increases significantly after the age of 40. This is particularly true for individuals who have a family history of clotting disorders or who have experienced surgery, trauma, or prolonged immobilization. Certain medical conditions, such as heart disease, cancer, and diabetes, can also increase the risk of blood clots at any age.
Understanding the elevated risk of blood clots with age is essential for taking precautionary measures. Maintaining a healthy lifestyle through regular exercise, a nutritious diet, and avoiding smoking can help reduce the risk. Regular medical checkups can also help identify any underlying conditions that may increase the likelihood of blood clots and allow for early intervention. By being aware of the risks and taking appropriate steps to mitigate them, individuals can enjoy a healthier and more fulfilling life as they age.
Identifying Risk Factors for Blood Clots
Age: As we age, our risk of developing blood clots increases. This is because our blood becomes thicker and our blood vessels may become damaged over time.
Smoking: Smoking damages the lining of blood vessels, making them more likely to develop clots. The nicotine in cigarettes also causes blood platelets to become stickier, increasing the risk of clot formation.
Obesity: Being overweight or obese increases your risk of blood clots because it can lead to increased levels of fatty acids in the blood, which can contribute to clot formation.
Pregnancy: During pregnancy, the body produces higher levels of estrogen, which can thicken the blood and increase the risk of clots. Additionally, the pressure of the growing uterus on the veins in the legs can also increase the risk of DVT.
Family history of clotting disorders: If you have a family history of blood clots, you are at an increased risk of developing them yourself. This is because blood clotting disorders can be inherited.
Identifying Risk Factors for Blood Clots
Age plays a pivotal role in the formation of blood clots. As we age, our blood vessels lose their elasticity, and blood flow slows down, making us more susceptible to clots.
Smoking is another significant risk factor. The chemicals in cigarettes damage the lining of your blood vessels, increasing the chances of plaque buildup and blood clots.
Obesity is also a contributing factor. Excess weight puts pressure on your veins, especially in the legs, leading to reduced blood flow and increased risk of clotting.
Pregnancy is another known risk factor. Hormonal changes during pregnancy make blood more prone to clotting. This risk is further amplified in the postpartum period.
A family history of clotting disorders is another non-modifiable risk factor. If you have a family member with a history of blood clots, you are more likely to develop them yourself. Genetic mutations can increase the activity of clotting proteins in your blood.
Understanding these risk factors is crucial for taking proactive measures to prevent blood clots. By making healthy lifestyle choices and consulting with your doctor if you have any underlying conditions, you can significantly reduce your risk.
Provide tips for reducing the risk of blood clots, including exercise, weight management, and avoiding prolonged inactivity.
**Preventing Blood Clots: Embracing a Healthier Lifestyle**
Blood clots, a serious health concern, can have life-threatening consequences. While certain medical conditions can increase your risk, making lifestyle changes can significantly reduce your chances of experiencing a clot. Here are a few simple tips to help you stay clot-free:
1. Embrace the Power of Movement
Regular exercise is an excellent way to keep your blood flowing and prevent clots from forming. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Brisk walking, swimming, cycling, and dancing are all great options.
2. Maintain a Healthy Weight
Obesity is a major risk factor for blood clots. Excess weight puts pressure on your veins, making it harder for blood to circulate properly. Aim for a healthy weight for your height and age.
3. Avoid Prolonged Inactivity
If you have to sit or stand for long periods, take frequent breaks to get up and move around. This helps keep your blood from pooling in your legs and feet. If you’re traveling, wear compression stockings to improve circulation.
Remember, preventing blood clots is all about making healthy choices. By incorporating these simple tips into your lifestyle, you can significantly reduce your risk and enjoy a healthier, more fulfilling life. If you have any concerns about your risk of blood clots, consult your doctor for personalized advice.
Understanding the Importance of Medical Checkups and Medication Adherence for Blood Clot Prevention
For individuals with underlying conditions that elevate their risk of developing blood clots, such as atrial fibrillation, valvular heart disease, or congestive heart failure, regular medical checkups are paramount. These appointments allow healthcare professionals to monitor the patient’s condition, assess their risk factors, and adjust their treatment plan if necessary.
During medical checkups, the doctor will typically perform a physical exam, review the patient’s medical history, and order blood tests to determine the coagulation profile. This profile measures the blood’s ability to clot and can help the doctor determine if the patient’s blood thinner dosage is appropriate.
Medication adherence is another crucial aspect of blood clot prevention. Blood thinners are effective only when taken as prescribed. Skipping doses or taking them at the wrong time can increase the risk of a blood clot forming. Patients should be instructed on proper medication administration and encouraged to use reminder systems or pill organizers to enhance adherence.
By adhering to their medication regimen and attending regular medical checkups, individuals with elevated clotting risk can significantly reduce their chances of developing a life-threatening blood clot. These preventive measures empower patients to take control of their health and safeguard their well-being.
Blood Clots: Recognizing the Warning Signs and Acting Swiftly
The sudden onset of pain, swelling, and throbbing in your leg could be more than just a muscle strain. It may be a silent assassin lurking within your veins, threatening to strike at any moment. A blood clot, a dangerous clump of solidified blood, can form in your deep veins, a condition known as deep vein thrombosis (DVT).
DVT can be treacherous because it often develops without any noticeable symptoms. However, certain warning signs can alert you to its presence:
- Pain, swelling, and tenderness in your leg or arm: These symptoms typically occur on one side of your body and worsen over time.
- Skin discoloration: Your skin may become red, blue, or purple around the affected area.
- Warmth: The area surrounding the clot may feel warm to the touch.
- Veins that appear swollen or bulgy: Raised, visible veins may indicate a blood clot blocking the flow of blood.
Pulmonary embolism (PE), a life-threatening complication of DVT, occurs when a blood clot travels through your veins and lodges in your lungs. The symptoms of PE can be sudden and severe:
- Sudden shortness of breath: You may experience difficulty breathing that develops rapidly.
- Chest pain: Pain or discomfort in your chest may accompany shortness of breath.
- Rapid heart rate: Your heart may race as it tries to compensate for the reduced blood flow to your lungs.
- Coughing up blood: In severe cases, you may cough up blood-tinged sputum.
Remember, time is of the essence when it comes to blood clots. If you experience any of these symptoms, seek immediate medical attention. Delay can increase the risk of serious complications, including organ damage or even death.
Blood Thinners: The Importance of Regular Blood Monitoring
Managing blood thinners is crucial for preventing blood clots. Regular blood monitoring is essential to ensure that the dosage is correct. This is because blood thinners can be tricky medications. Too much can lead to excessive bleeding, while too little may not be enough to prevent clots.
Blood monitoring helps doctors adjust the dosage to optimize the balance between preventing clots and minimizing bleeding risks. The frequency of monitoring varies depending on the type of blood thinner and individual factors. For example, warfarin (Coumadin) requires more frequent monitoring than newer blood thinners like apixaban and rivaroxaban.
During blood monitoring, a blood sample is taken to measure the prothrombin time (PT) or activated partial thromboplastin time (aPTT). These tests assess how quickly your blood clots. The results help determine if the blood thinner dosage is appropriate.
Regular monitoring also allows doctors to detect any changes in your clotting behavior or interact with other medications you’re taking. This helps ensure that your blood thinner treatment remains effective and safe.
If you’re taking blood thinners, it’s essential to follow your doctor’s instructions for regular blood monitoring. This monitoring is a vital part of managing your condition and staying healthy.
Managing Blood Thinners: Essential Lifestyle Adjustments
Taking blood thinners is crucial for preventing and treating blood clots. However, to ensure their effectiveness and minimize potential adverse effects, certain lifestyle adjustments are essential.
Avoiding Interfering Medications
Some medications can interact with blood thinners, reducing their efficacy or increasing the risk of bleeding. These include nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen, as well as antibiotics like ciprofloxacin and clarithromycin. Always consult your doctor before taking any other medications while on blood thinners.
Dietary Modifications
Certain foods contain vitamin K, which can decrease the effectiveness of blood thinners. Foods rich in vitamin K include leafy green vegetables (e.g., spinach, kale), broccoli, Brussels sprouts, and soybeans. While it’s important to maintain a healthy diet, limiting the intake of these foods or consuming them consistently can help ensure stable blood thinner levels.
Avoiding Alcohol and Smoking
Alcohol can increase the risk of bleeding, especially when combined with blood thinners. While moderate alcohol consumption may be allowed, it’s best to consult your doctor for specific guidelines. Smoking also increases clotting risk and can interact with blood thinners, so it’s strongly advised to quit smoking.
Regular Monitoring and Communication
Regular blood tests are crucial for monitoring blood thinner levels. By consistently checking your blood, your doctor can ensure that your dosage is optimized, reducing the risk of both clots and bleeding. Open communication with your healthcare provider is vital to address any concerns or adjust medications as needed.
By following these lifestyle adjustments, you can maximize the effectiveness of your blood thinners, minimize potential complications, and maintain good overall health. Remember to consult your doctor regularly and prioritize your well-being.
Provide tips for minimizing the risk of bleeding and bruising associated with blood thinners.
Minimizing Bleeding and Bruising with Blood Thinners
Taking blood thinners is crucial for preventing dangerous blood clots. However, it’s essential to manage them properly to minimize the risk of excessive bleeding and bruising. Here are some practical tips to help you stay safe:
Monitor Your Diet Wisely:
- Limit Vitamin K Intake: Vitamin K promotes blood clotting, so it’s vital to be mindful of your intake. Leafy greens, such as spinach and kale, are rich in vitamin K, so consume them in moderation.
- Avoid Alcohol: Alcohol can interact with blood thinners and increase the risk of bleeding. It’s best to limit alcohol consumption or abstain from it altogether.
Be Cautious with Medications:
- Inform Healthcare Providers: Always disclose your blood thinner usage to your doctor and pharmacist. Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, can interfere with blood thinners and increase bleeding risk.
- Check Medication Interactions: Use a reputable drug interaction checker or consult with your pharmacist to identify potential interactions between your blood thinners and other medications you may be taking.
Lifestyle Adjustments:
- Avoid Contact Sports: Sports involving physical contact can increase the risk of falls and injuries, which could lead to excessive bleeding. Consider safer activities like swimming or walking instead.
- Use Electric Razors: Electric razors are gentler on the skin than traditional razors, reducing the likelihood of cuts and bruises.
- Wear Compression Stockings: Compression stockings can help prevent blood clots in the legs and minimize the risk of bruising.
Other Precautions:
- Regular Blood Monitoring: Regular blood tests are essential to ensure your blood thinner dosage is correct and effective. Follow your doctor’s instructions for monitoring appointments.
- Report Unusual Symptoms: Pay attention to any unusual symptoms, such as prolonged bleeding, unexplained bruising, or dizziness. Report these promptly to your healthcare provider for prompt medical attention.
- Carry an ID Card: Carrying a medical ID card that states you’re taking blood thinners can alert medical professionals in an emergency situation.
Minimizing bleeding and bruising while taking blood thinners is crucial for your well-being. By following these practical tips, you can reduce the risks and improve your quality of life. Remember, always consult with your doctor or pharmacist for personalized guidance and to ensure you’re getting the best and safest care.