Rabies In Dogs: Symptoms, Prevention, And Treatment For Optimal Health
Recognizing rabies in dogs requires observing changes in behavior and physical symptoms. Unusual aggression, paralysis, difficulty breathing or swallowing, and digestive problems can indicate rabies. The rabies virus, transmitted through bites and scratches, affects the nervous system. Prevention involves vaccination, animal control, and bite avoidance. Diagnosis relies on laboratory tests, while treatment involves post-exposure prophylaxis to prevent infection spread. Understanding rabies symptoms and prevention measures helps ensure public health and minimizes the risk of transmission.
Rabies: A Deadly Threat to Humans and Animals
Rabies, a fatal viral disease, has plagued humanity for centuries. Recognizing its significance as a public health concern is crucial. Understanding the disease can empower us to protect ourselves and our communities from this deadly virus.
Rabies: The Deadly Virus
Rabies, caused by the rabies virus, is a neurological disease that attacks the central nervous system. Once infected, the virus can spread to the brain, leading to a range of devastating symptoms.
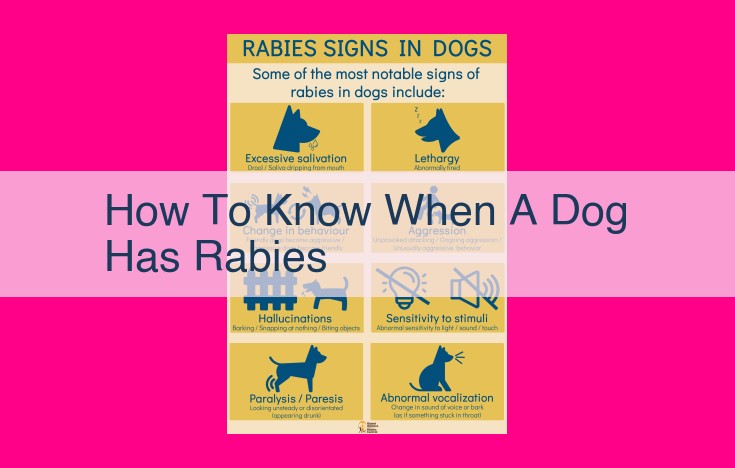
Symptoms of Rabies
The manifestations of rabies can vary depending on the stage of the disease. Early symptoms may include fever, malaise, and headache. As the virus progresses, more severe symptoms emerge:
- Neurological Symptoms: Aggression, paralysis, hydrophobia (fear of water)
- Respiratory Symptoms: Shortness of breath, difficulty swallowing
- Digestive Symptoms: Vomiting, diarrhea, abdominal pain
Transmission of Rabies
Rabies is primarily transmitted through the bite of infected animals, such as dogs, cats, and bats. The virus can also be spread through contact with the saliva or other bodily fluids of an infected animal.
Prevention of Rabies
Vaccination: Vaccination is the cornerstone of rabies prevention. It provides protection against the virus for both humans and animals.
Animal Control: Effective animal control measures, including stray animal management and vaccination programs, reduce the risk of rabies transmission from animals to humans.
Bite Prevention: Avoiding contact with animals, especially stray or wild animals, is crucial. If bitten or scratched by an animal, seek immediate medical attention.
Diagnosis and Treatment of Rabies
Diagnosis: Confirming rabies requires laboratory testing, such as antigen detection and antibody testing.
Treatment: There is no cure for rabies once symptoms develop. However, post-exposure prophylaxis (PEP), a combination of wound cleaning, rabies immune globulin, and rabies vaccine, can prevent the onset of the disease if administered promptly after exposure.
Public Health and Rabies
Rabies surveillance and reporting are essential for tracking the disease and preventing outbreaks. Public education and awareness campaigns empower individuals to take responsibility for rabies prevention.
Research on Rabies
Ongoing research focuses on improving rabies vaccines and developing new treatment options. Understanding animal reservoirs of rabies is also crucial for effective rabies control.
Key Organizations Involved in Rabies Control
- Centers for Disease Control and Prevention (CDC): Surveillance, prevention, and response
- World Health Organization (WHO): Global vaccination campaigns and collaboration
- Animal Control Agencies: Outbreak prevention and stray animal management
- Veterinary Clinics: Diagnosis, treatment, and prevention guidance
The Frightening Symptoms of Rabies: A Tale of Neurological, Respiratory, and Digestive Distress
Rabies, a deadly viral infection that primarily affects the nervous system, is a cause of great concern for public health. The disease manifests through an array of symptoms, ranging from subtle neurological changes to severe respiratory and digestive distress.
Neurological Symptoms: When the Brain Under Attack
- Aggression: Rabies can trigger sudden and unprovoked aggression in individuals, even those typically gentle.
- Paralysis: As the virus spreads through the nervous system, paralysis can develop, affecting limbs and even the face.
- Hydrophobia: One of the most distinctive symptoms of rabies is the fear of water, caused by spasms in the throat and esophagus.
Respiratory Symptoms: Struggling for Breath
- Shortness of breath: Rabies can cause inflammation and swelling in the airways, making breathing difficult.
- Difficulty swallowing: Paralysis of the throat muscles can hinder swallowing, leading to choking and aspiration.
Digestive Symptoms: Disruptions in the Gut
- Vomiting: The virus can irritate the digestive tract, causing frequent vomiting.
- Diarrhea: Diarrhea, often bloody, can occur as a result of gastrointestinal inflammation.
- Abdominal pain: Severe abdominal pain can be a sign of rabies’s impact on the digestive system.
These symptoms of rabies underscore the severity of this disease and the urgent need for proper diagnosis and treatment. Early recognition and intervention are crucial to improve outcomes and potentially save lives.
The Etiology of Rabies: Unraveling the Pathogenesis of a Deadly Virus
Introduction:
Rabies, a dreaded disease that has plagued humanity for centuries, is caused by the insidious rabies virus. Understanding the nature and behavior of this virus is crucial for effective prevention and treatment strategies.
Rabies Virus: The Evil Within
The rabies virus, a lyssavirus belonging to the Rhabdoviridae family, is a formidable foe. Its elongated, bullet-shaped structure conceals a complex genome that encodes an array of deadly proteins. These proteins, such as the glycoprotein G, facilitate the virus’s entry into host cells and its subsequent takeover of the nervous system.
Mechanism of Action: A Stealthy Attack on the Nervous System
Once inside host cells, the rabies virus hijacks their machinery to replicate its genome and produce new viral particles. These particles then embark on a stealthy journey along the victim’s nervous system, exploiting the nerve endings as highways to reach the central nervous system. As the virus infiltrates the brain and spinal cord, it causes severe inflammation and damage, triggering the characteristic symptoms of rabies.
The Viral Nightmare: Neurological Mayhem
The rabies virus’s assault on the nervous system manifests in a range of devastating neurological symptoms. Paralysis, caused by viral damage to the motor neurons, gradually robs the victim of mobility. Hydrophobia, a hallmark symptom, results from the virus’s disruption of brain centers controlling swallowing, making it excruciating for victims to drink water. Other neurological manifestations include hallucinations, seizures, and progressive coma.
Epidemiology and Transmission of Rabies:
- Transmission: Explain how rabies is transmitted from animals to humans and the role of bites and scratches in transmission.
Epidemiology and Transmission of Rabies
Rabies, a deadly viral disease, is primarily transmitted from animals to humans through bites or scratches. Infected animals, such as bats, dogs, and raccoons, carry the virus in their saliva. During a bite, the virus can enter the human body through the wound and travel to the central nervous system, causing severe neurological symptoms.
The transmission of rabies can occur in various settings. Wild animals, such as bats, skunks, and foxes, can transmit the virus to humans through bites or scratches during encounters in forests or caves. Domestic animals, primarily dogs and cats, play a significant role in rabies transmission, particularly in regions where vaccination programs are not widely implemented. These animals can contract rabies from infected wildlife and then pass it on to humans through bites.
Understanding the epidemiology and transmission of rabies is crucial for effective prevention strategies. Avoiding contact with wild animals, especially bats, is essential. Vaccinating domestic animals and implementing animal control measures can significantly reduce the risk of rabies transmission. Additionally, practicing proper wound care and seeking immediate medical attention after any animal bite are vital steps in preventing rabies infection.
Prevention of Rabies: A Crucial Step to Stay Safe
Rabies, a deadly viral infection, is a global health concern. However, prevention is paramount in combating this disease.
Vaccination: The Primary Defense
The most effective way to prevent rabies is through vaccination. It stimulates the immune system to recognize and fight the rabies virus, protecting individuals from the deadly infection. Pre-exposure vaccination is recommended for people with high-risk occupations, travelers to rabies-endemic areas, and those who live in close proximity to wild animals.
Animal Control: Managing the Reservoirs
Rabies is primarily transmitted through the bites of infected animals. Therefore, animal control plays a crucial role in rabies prevention. By controlling the population of stray animals, especially dogs and cats, the likelihood of contact between humans and infected animals is reduced. Vaccinating domestic animals and implementing spaying and neutering programs are essential to contain the spread of rabies.
Bite Prevention: Avoiding Risky Encounters
To prevent rabies, it is vital to avoid animal bites and scratches. Avoid approaching unfamiliar animals, even if they appear friendly. If bitten or scratched, it is imperative to clean the wound thoroughly with soap and water and seek immediate medical attention. Delay in seeking treatment can have dire consequences.
Remember, rabies is a deadly but preventable disease. By embracing these preventive measures – vaccination, animal control, and bite prevention – you can significantly reduce your risk of infection and protect both yourself and your community. Stay informed, take precautions, and spread awareness to combat rabies effectively.
Diagnosis of Rabies: Unraveling the Enigma
Laboratory Testing: The Key to Unlocking the Mystery
Confirming a rabies infection requires a meticulous approach, and laboratory testing plays a pivotal role in this process. Rabies virus antigen detection and antibody testing are the cornerstones of rabies diagnosis, providing definitive evidence of the virus’s presence or the immune response it triggers.
Rabies Virus Antigen Detection: Seeking the Virus’s Traces
Rabies virus antigen detection involves isolating and identifying specific proteins associated with the rabies virus. These proteins, called antigens, are like fingerprints of the virus, allowing scientists to pinpoint its presence in a sample. The fluorescent antibody technique is commonly employed for this purpose, where antibodies tagged with a fluorescent dye bind to rabies antigens, revealing their location under a microscope.
Antibody Testing: Detecting the Body’s Response
Antibody testing, on the other hand, measures the levels of antibodies produced by the body’s immune system in response to the rabies virus. Neutralizing antibody testing is a crucial technique that determines the individual’s capacity to neutralize (inactivate) the rabies virus. High levels of neutralizing antibodies indicate a robust immune response and a lower risk of rabies development.
Time is of the Essence: The Importance of Early Diagnosis
Time is of paramount importance in diagnosing rabies. Early detection and prompt treatment can significantly increase the chances of survival. If you suspect rabies infection, it is imperative to seek medical attention immediately. A delay in diagnosis can have dire consequences, as rabies is a fatal disease if left untreated.
Collaborating Efforts: A Collective Approach to Rabies Diagnosis
Rabies diagnosis requires a collaborative effort among various healthcare professionals. Physicians, veterinarians, and laboratory technicians work together to interpret test results and determine the appropriate course of action. The accuracy and reliability of diagnostic tests are paramount in ensuring timely and effective rabies management.
Treating Rabies: A Lifeline After the Bite
Rabies, a deadly viral infection transmitted through animal bites, has historically instilled fear and dread. However, post-exposure prophylaxis (PEP) offers a glimmer of hope in the face of this formidable disease. PEP is a crucial intervention that can prevent rabies from taking hold after a potential exposure.
After a bite or scratch from an animal suspected of rabies, immediate wound cleaning is paramount. This helps remove the virus from the wound site and reduces the risk of infection. Next, rabies immune globulin (RIG) is administered. RIG contains antibodies that neutralize the rabies virus and prevent it from establishing itself in the body.
Finally, a series of rabies vaccines is given to boost the body’s own immune response against rabies. These vaccines are highly effective in preventing the development of the disease, provided they are administered promptly after exposure.
The importance of PEP cannot be overstated. In countries where rabies is endemic, PEP has significantly reduced the number of human rabies cases. It is essential to seek medical attention immediately after any potential rabies exposure to ensure the timely administration of PEP.
Early diagnosis and prompt treatment are critical for rabies. PEP provides a vital lifeline after a potential rabies exposure, preventing the devastating consequences of this deadly disease.
Public Health and Rabies: A Collaborative Effort
Rabies, a fatal viral disease, poses a significant threat to public health worldwide. To effectively combat this disease, robust surveillance and comprehensive education campaigns play a vital role.
Surveillance: Tracking the Trail of Rabies
Surveillance is the backbone of rabies control. By closely monitoring animal populations and swiftly identifying cases, public health officials can promptly respond to outbreaks and prevent further spread. Surveillance involves actively searching for rabid animals, collecting samples for laboratory testing, and tracking trends in rabies cases. This information enables health authorities to assess the risk to humans and implement targeted interventions.
Education and Awareness: Empowering Communities
Public education and awareness are crucial for rabies prevention. By informing individuals about the risks and symptoms of rabies, as well as the importance of preventive measures, communities can become active partners in safeguarding their health. Education campaigns should emphasize the role of vaccination, responsible animal ownership, and immediate medical attention in case of animal bites or scratches. By empowering communities with knowledge, public health officials can significantly reduce the risk of rabies transmission and protect vulnerable populations.
Unveiling the Mysteries of Rabies: A Comprehensive Guide
Rabies, an ancient and deadly disease, continues to pose a significant public health threat worldwide. It’s imperative to understand its nature, symptoms, and preventive measures to safeguard our communities from this lethal adversary.
Symptoms: A Chilling Spectrum of Distress
The manifestation of rabies is a haunting array of neurological, respiratory, and digestive symptoms. Aggression, paralysis, and hydrophobia are telltale signs that strike fear in the hearts of those affected. Shortness of breath and difficulty swallowing add to the torment, while vomiting, diarrhea, and abdominal pain further burden the body.
Etiology: The Rabies Virus Exposed
The culprit behind rabies is a virus of cunning complexity. Its cylindrical form harbors a genetic code that wreaks havoc on the nervous system, causing irreversible damage. Understanding the virus’s structure and mechanisms of action is crucial for developing effective countermeasures.
Epidemiology and Transmission: Breaking the Chain of Infection
Rabies is primarily transmitted through the bites and scratches of infected animals, with dogs serving as the most common source. Comprehending the mode of transmission empowers individuals with the knowledge to avoid contact with potentially rabid animals.
Prevention: Pillars of Protection
Vaccination stands as the cornerstone of rabies prevention. Animal control plays a vital role in managing stray animals and preventing outbreaks. Educating the public about bite avoidance techniques further strengthens our defenses against this deadly disease.
Diagnosis: Unraveling the Mystery
Confirming a rabies diagnosis requires laboratory testing, including rabies virus antigen detection and antibody testing. These tests provide invaluable information, allowing healthcare professionals to make timely decisions and initiate appropriate treatment.
Treatment: A Race Against Time
Post-exposure prophylaxis is the lifesaving lifeline for individuals who have come into contact with a potentially rabid animal. Wound cleaning, rabies immune globulin, and rabies vaccine form the foundation of this critical treatment protocol.
Public Health and Rabies: A Collaborative Effort
Surveillance and reporting are essential for tracking rabies cases and preventing outbreaks. Public education and awareness campaigns empower communities to recognize and report potential exposures.
Research on Rabies: Pushing the Boundaries of Knowledge
Unceasing research efforts drive the development of improved rabies vaccines and treatment options. Understanding the animal reservoirs of the virus is vital for implementing effective control strategies.
Key Organizations Involved in Rabies Control
The Centers for Disease Control and Prevention (CDC) leads the charge in surveillance, prevention, and response to rabies. The World Health Organization (WHO) spearheads global initiatives, promoting vaccination campaigns and collaboration. Animal control agencies and veterinary clinics play indispensable roles in preventing outbreaks and managing stray animals.
Key Organizations Involved in Rabies Control
Rabies is a deadly disease that affects both humans and animals. Understanding the roles of key organizations in rabies control is crucial for preventing and combating this disease.
Centers for Disease Control and Prevention (CDC)
The CDC is a leading authority in public health, playing a vital role in rabies surveillance, prevention, and response. The organization collects and analyzes data on rabies cases, providing valuable insights into the disease’s distribution and trends. The CDC also develops and disseminates guidelines for rabies prevention and control, ensuring that healthcare providers and the public have access to the most up-to-date information.
World Health Organization (WHO)
The WHO coordinates global efforts to combat rabies, with a focus on vaccination campaigns and collaboration. The organization provides technical assistance to countries to strengthen their rabies control programs, including support for vaccine procurement, surveillance systems, and education initiatives. The WHO also works to raise awareness about rabies and advocate for increased funding and resources for rabies control worldwide.
Animal Control Agencies
Animal control agencies are essential in preventing rabies outbreaks and managing stray animals. These agencies work to identify and vaccinate stray animals, reducing the risk of transmission to humans and other animals. Animal control officers also investigate animal bite reports, assess the risk of rabies exposure, and provide guidance on post-bite care.
Veterinary Clinics
Veterinary clinics play a crucial role in diagnosing and treating rabies cases. Veterinarians can perform laboratory tests to confirm a rabies infection and provide appropriate treatment, including wound cleaning, rabies immune globulin, and rabies vaccine. They also provide guidance on rabies prevention measures, such as vaccination and avoiding contact with wild animals.