Effective Non-Surgical And Surgical Solutions To Vanish Under-Eye Veins
To reduce the appearance of under-eye veins (telangiectasia), consider non-surgical options like laser therapy, sclerotherapy, microneedling, and topical treatments containing green tea or horse chestnut extracts. Non-invasive approaches include cold compresses or oral supplements. Consult a healthcare professional for personalized treatment advice, such as filler injections or surgical interventions, if necessary.
Tackling Telangiectasia and Periorbital Hyperpigmentation: Your Comprehensive Guide to Treatment
Ever wondered what those tiny, visible blood vessels or dark patches around your eyes are? They’re called telangiectasia and periorbital hyperpigmentation, and they can affect your confidence.
But fear not! This blog post has your back. We’ll delve into the causes of these conditions and empower you with a * comprehensive overview of treatment options*, helping you achieve your desired clear and radiant skin.
Etiology of Telangiectasia and Periorbital Hyperpigmentation
Understanding the causes of telangiectasia and periorbital hyperpigmentation is crucial for developing effective treatment strategies. These conditions, often seen on the face, share common underlying factors that contribute to their development.
Venous Insufficiency
Venous insufficiency is a condition where the veins are unable to adequately drain blood from the body. This can lead to the formation of enlarged, twisted veins known as varicose veins. Varicose veins can weaken the tiny blood vessels called capillaries, causing them to expand and become visible under the skin, resulting in telangiectasia.
Varicose Veins
Varicose veins are a common cause of telangiectasia, especially around the legs and face. The pressure exerted by the enlarged veins damages the capillaries, making them more fragile and prone to dilation. This results in the development of visible spider veins on the surface of the skin.
In addition to venous insufficiency, other factors can contribute to telangiectasia and periorbital hyperpigmentation. These include sun exposure, aging, hormonal changes, and certain medical conditions. Understanding these underlying causes is essential for determining the most appropriate treatment approach for each individual.
Risk Factors for Telangiectasia and Periorbital Hyperpigmentation
Age
As we gracefully navigate through the chapters of life, our skin undergoes a natural aging process. With time, the delicate tissues surrounding our eyes become more vulnerable to telangiectasia and periorbital hyperpigmentation. The skin thins, and the collagen and elastin fibers that provide support weaken. This age-related decline in skin integrity makes it more susceptible to the development of these conditions.
Sun Exposure
Soaking up the sun’s rays may bring temporary joy, but prolonged exposure can take a toll on our delicate skin. Ultraviolet radiation damages the blood vessels and melanocytes, contributing to the formation of telangiectasia and hyperpigmentation. Repeated exposure to the sun’s harmful rays can worsen these conditions, highlighting the importance of sun protection in preserving our skin’s health.
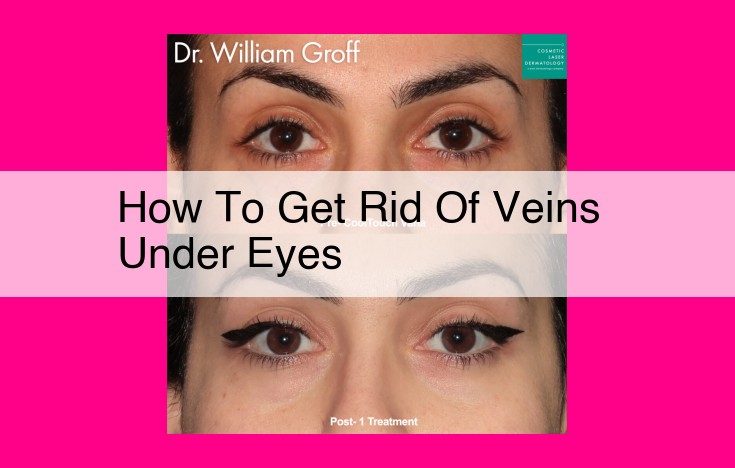
Treatment Options for Managing Telangiectasia and Periorbital Hyperpigmentation
The journey to a brighter and more even complexion can be challenging when faced with telangiectasia and periorbital hyperpigmentation. However, professional medical advice can guide you towards personalized treatment options to restore your confidence.
Non-Surgical Approaches:
-
Laser Therapy: With precise beams of light, laser therapy targets the damaged or discolored blood vessels. The energy seals them off, reducing their visibility.
-
Sclerotherapy: Tiny injections of a chemical solution are used to collapse and fade unsightly veins. This technique works well for telangiectasia on the face.
-
Microneedling: Microscopic needles create tiny channels in the skin, stimulating collagen production and reducing the appearance of pigmentation and dilated vessels.
-
Chemical Peels: Superficial or deep peels exfoliate the skin’s outer layers, revealing brighter, more uniform skin. They can address periorbital hyperpigmentation.
-
Platelet-Rich Plasma Injections: A concentration of the patient’s own platelets is injected, stimulating skin rejuvenation and improving discoloration.
-
Cold Compresses: Regularly applying cold compresses can constrict blood vessels, making telangiectasia less noticeable.
Topical Remedies:
-
Green Tea Extract: This antioxidant can reduce inflammation and soothe irritated skin. Its anti-inflammatory properties help improve periorbital hyperpigmentation.
-
Horse Chestnut Extract: A natural anti-inflammatory, it strengthens and repairs blood vessel walls, reducing their visibility.
-
Witch Hazel: Astringent and antibacterial, it tones the skin and reduces swelling. It can lighten dark circles and constrict telangiectasia.
-
Cucumbers: Rich in water and antioxidants, cucumbers hydrate and brighten the skin. Placing cucumber slices on the affected areas can reduce inflammation and discoloration.
-
Vitamin K Cream: Applied topically, this vitamin strengthens fragile blood vessels and improves their appearance.
Oral Supplements:
- Vitamin C Supplements: As an essential nutrient, vitamin C aids in collagen production, protecting the skin from damage. It can help reduce periorbital hyperpigmentation.
Cosmetic Procedures:
-
Filler Injections: Hyaluronic acid fillers can temporarily plump the skin, reducing the appearance of under-eye hollows that contribute to periorbital hyperpigmentation.
-
Camouflage Makeup: Concealers and color-correctors can effectively camouflage telangiectasia and hyperpigmentation, offering instant but temporary coverage.
Surgical Intervention:
- Surgery: In severe cases, surgery may be necessary to remove enlarged veins or correct underlying conditions causing telangiectasia and periorbital hyperpigmentation.
Remember, individual treatment plans may vary depending on the severity of the condition, its underlying cause, and the patient’s overall health. Consulting a board-certified dermatologist or a qualified healthcare professional is crucial for personalized advice and effective treatment options. Embark on this journey with confidence, knowing that professional guidance will lead you towards a brighter, healthier complexion.