Mosaic Embryos: Genetic Complexities And Implications For Fertility Treatments
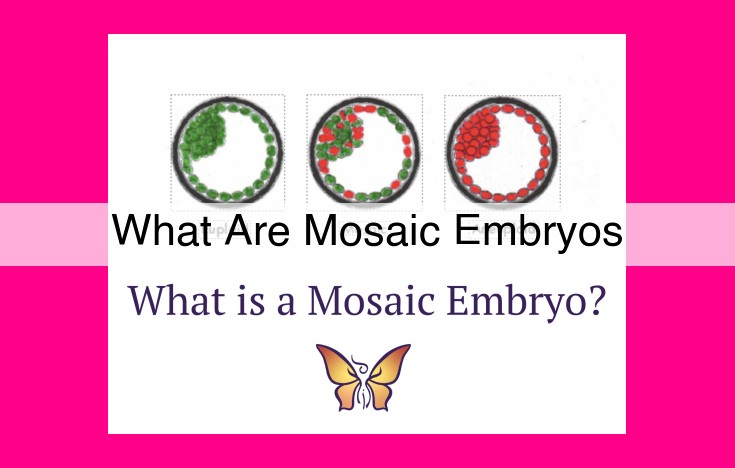
Mosaic embryos occur when an individual has multiple cell lines with different genetic compositions. This phenomenon can result from genetic mutations or technical errors in fertility treatments such as in vitro fertilization (IVF) or preimplantation genetic testing (PGT). Mosaic embryos pose unique challenges in genetic testing and counseling, as their genetic makeup can vary across different cells within the embryo.
Mosaicism: A Tale of Genetic Diversity Within One Body
Imagine a vibrant mosaic, where each tile represents a unique genetic code. Mosaicism, a fascinating biological phenomenon, is like this colorful masterpiece, where different cell lines within a single individual possess distinct genetic compositions.
Unlike a standard mosaic, where each tile is meticulously placed, mosaicism arises spontaneously. During early embryonic development, a genetic mutation occurs in a single cell. This mutated cell then divides, giving rise to a clonal population of cells that carry the same genetic variation. Intriguingly, these genetically altered cells can coexist alongside normal cells, forming a mosaic pattern within the individual’s body.
The origin of mosaicism can be traced back to various events. It can arise during fertilization, when two sperm cells fuse with the same egg, resulting in a triploid embryo. Alternatively, it can occur during early embryonic development, when a rare event known as chromosomal nondisjunction results in an abnormal number of chromosomes in a particular cell.
Mosaic individuals may display a wide range of physical and health implications, depending on the nature and location of their genetic variation. Some individuals may experience subtle or no symptoms, while others may exhibit more pronounced features. Mosaicism can also affect different cell types, leading to a mosaic pattern of symptoms or traits.
Understanding mosaicism is crucial for both scientific research and clinical practice. By unraveling the genetic complexities of mosaicism, researchers can gain insights into the fundamental processes of human development and disease susceptibility. Clinicians, on the other hand, can utilize this knowledge to provide tailored care and genetic counseling to individuals with mosaic conditions.
**Chimerism: A Rare but Fascinating Genetic Phenomenon**
Unraveling the Enigma of Chimerism:
Chimerism is a remarkable occurrence in biology that happens when two or more separate zygotes (fertilized eggs) merge during pregnancy, resulting in a single individual with distinct genetic material in different parts of their body. Imagine if two embryos decided to cozy up and become roommates, sharing space and resources.
Fusion and Fellowship:
The formation of a chimera is akin to a biological fusion, where the cells from each embryo intermingle and coexist peacefully. However, unlike the harmonious blending of two different cuisines, chimerism can lead to a mosaic of genetic diversity within the same body. Imagine each embryo as a different-colored paint, merging to create a vibrant patchwork of genetic hues.
Cells with Separate Identities:
Within a chimera, each cell retains its unique genetic makeup, a testament to its original embryo. So, you could have cells with different sets of chromosomes, each containing a distinct genetic blueprint. It’s like having a genetic library with multiple volumes, each telling a different story.
Chimerism in Nature:
Chimerism is not exclusive to humans; it’s found in a variety of animals, including cats, dogs, cows, and even plants. Nature has a way of producing these genetic mash-ups, adding an extra layer of complexity to the tapestry of life.
Trisomy 21: Understanding Down Syndrome
Nestled within our genetic code lies an intricate dance of chromosomes, each carrying a unique blueprint for our lives. But sometimes, an unexpected guest joins the party – an extra copy of chromosome 21. This chromosomal anomaly is known as Trisomy 21, or more commonly, Down Syndrome.
Down Syndrome is a genetic condition that affects individuals in both physical and cognitive ways. It’s a story of genetic variation that has captivated the medical community and touched the lives of countless families.
Causes and Development
The journey of Down Syndrome begins during conception, when an error in cell division leads to an additional copy of chromosome 21. This can occur in one of two ways:
- Nondisjunction: During meiosis, when sperm or egg cells are formed, a pair of chromosomes fails to separate properly, resulting in one gamete carrying an extra copy.
- Robertsonian Translocation: A fragment of chromosome 21 attaches to another chromosome, leading to an extra full or partial copy of chromosome 21.
Physical and Cognitive Characteristics
Each individual with Down Syndrome carries their unique tapestry of strengths and challenges. Physical characteristics may include:
- Distinctive facial features: Smaller nose, upturned eyes, and a rounder face
- Short stature
- Hypotonia (low muscle tone)
- Congenital heart defects
Cognitive development often progresses at a slower pace, leading to challenges in learning, memory, and problem-solving. However, individuals with Down Syndrome often display remarkable strengths in areas such as social skills, empathy, and creativity.
Trisomy 18 (Edwards Syndrome): Describe this genetic condition, its causes, symptoms, and prognosis.
Trisomy 18: Breaking Down the Complex Genetic Condition
Understanding Trisomy 18
Trisomy 18, also known as Edwards Syndrome, is a rare genetic disorder caused by the presence of an extra copy of chromosome 18. This chromosomal abnormality occurs during cell division, resulting in a disrupted genetic balance. Individuals with Trisomy 18 face various challenges and require specialized medical care and support.
Causes and Prevalence
Approximately 1 in 5,000 pregnancies are affected by Trisomy 18. The exact cause remains unknown, but it’s believed to be a random event during cell division. Maternal age is not a significant risk factor, unlike other chromosomal disorders.
Symptoms and Prognosis
Symptoms of Trisomy 18 can vary widely, but common features include distinctive facial characteristics, delayed growth, and organ abnormalities. Affected infants may have a prominent forehead, flattened nose, narrow eyes, and low-set ears. Developmental delays, feeding difficulties, and heart defects are also common.
Trisomy 18 carries a serious prognosis. Most infants with this condition do not survive beyond their first year of life. Those who do may experience significant health challenges, requiring continuous medical care and special assistance.
Management and Support
Managing Trisomy 18 involves a multidisciplinary approach. Medical specialists, including geneticists, cardiologists, and developmental pediatricians, collaborate to provide comprehensive care. Treatment modalities focus on alleviating symptoms, improving quality of life, and providing palliative support.
Prenatal Diagnosis and Genetic Counseling
Prenatal testing methods, such as amniocentesis, can detect Trisomy 18 during pregnancy. If a diagnosis is made, genetic counseling plays a crucial role in providing information and support to prospective parents. Genetic counselors can discuss the condition, prognosis, and offer guidance on reproductive decisions.
Research and Future Directions
Ongoing research in genetics aims to improve our understanding of Trisomy 18. Scientists are exploring novel therapies, including gene editing and targeted treatments, to mitigate the effects of this disorder. The ultimate goal is to enhance the lives and outcomes of individuals affected by Trisomy 18.
Diagnostic Procedures: Shedding Light on Genetic Variations
Prenatal testing plays a crucial role in detecting genetic variations that can affect the health of an unborn child. Among the various methods available, three notable procedures stand out: Preimplantation Genetic Testing (PGT), Chorionic Villus Sampling (CVS), and Amniocentesis.
Preimplantation Genetic Testing (PGT):
PGT is an advanced technique performed on embryos created through In Vitro Fertilization (IVF) before they are implanted into the uterus. A small sample of cells is taken from the embryo and analyzed for genetic abnormalities, allowing parents to select embryos with the desired genetic profile. This procedure is often used to prevent the transmission of genetic disorders to future generations.
Chorionic Villus Sampling (CVS):
CVS is a diagnostic procedure that involves collecting cells from the chorionic villi, finger-like projections of the placenta. The procedure is performed transvaginally or transabdominally under ultrasound guidance. The cells are then analyzed for genetic abnormalities. CVS can be done as early as 10 weeks of pregnancy, providing earlier results compared to other prenatal tests.
Amniocentesis:
Amniocentesis is a procedure in which a small amount of amniotic fluid is withdrawn from the amniotic sac surrounding the fetus. The fluid contains fetal cells that can be analyzed for genetic variations. Amniocentesis is typically performed between 15 and 20 weeks of pregnancy and is considered a highly accurate test.
These prenatal testing methods empower expectant parents with valuable information about the genetic health of their unborn child. By understanding the risks and benefits associated with each procedure, individuals can make informed decisions regarding their reproductive choices.
Understanding the Roles of Geneticists and Genetic Counselors
Geneticists:
- Specialized physicians who have received extensive training in medical genetics and research.
- Diagnose and manage genetic conditions, such as Trisomy 21 and Trisomy 18.
- Conduct prenatal testing to identify genetic variations before birth.
Genetic Counselors:
- Allied health professionals with master’s degrees in genetic counseling.
- Provide support and education to patients and families before, during, and after genetic testing.
- Help patients understand the potential consequences of genetic variations and make informed decisions about their healthcare.
The Patient-Centered Collaboration:
Geneticists and genetic counselors work closely together to provide patients with comprehensive care. Geneticists use their medical expertise to diagnose and treat genetic conditions, while genetic counselors provide emotional support, education, and guidance.
This collaboration ensures that patients:
- Receive accurate information about their genetic variations.
- Understand the implications of these variations on their health and family planning.
- Make informed decisions about their treatment options and reproductive choices.
By working together, geneticists and genetic counselors empower patients with the knowledge and support they need to navigate the complex world of genetic conditions.
Reproductive Rights: The Ethical Labyrinth of Genetic Testing and Pregnancy
Understanding the Complexities
Genetic testing has emerged as a powerful tool in the realm of medicine, offering invaluable insights into our genetic makeup. However, as we delve deeper into the intricacies of DNA, we cannot overlook the ethical dilemmas that arise at the intersection of genetic testing and reproductive rights.
The Reproductive Autonomy Debate
The fundamental question that lies at the heart of this ethical quandary is: Should individuals have the right to make autonomous decisions regarding their own reproductive health, even if those decisions are influenced by genetic information?
Genetic testing can provide expectant parents with a wealth of information about potential risks and challenges associated with their unborn child. While this knowledge can be empowering, it also poses complex choices that can have profound implications for their family’s future.
Ethical Considerations of Choice
Some argue that individuals have a fundamental right to choose whether or not to have children based on genetic information. They believe that reproductive autonomy should prevail, regardless of the potential consequences. Others, however, contend that the potential impact on the child’s well-being should be paramount in decision-making.
Balancing Rights and Responsibilities
Striking a balance between individual rights and the well-being of potential children is a delicate task. As a society, we must engage in thoughtful and compassionate dialogue to navigate this ethical minefield. It is essential that we approach these decisions with empathy and a deep respect for the complexities of human life.
The Role of Genetic Counselors
Genetic counselors play a crucial role in facilitating this dialogue. They provide comprehensive information about genetic testing, its implications, and the potential choices available to prospective parents. Their expertise helps individuals make informed decisions that align with their values and aspirations.
The ethical implications of genetic testing on reproductive rights are vast and multifaceted. As we continue to advance our understanding of genetics, it is imperative that we approach these complex issues with open minds, compassionate hearts, and a unwavering commitment to upholding the autonomy and well-being of all individuals.
Patient Autonomy: Respecting the Power of Individual Choice in Healthcare
Within the intricate tapestry of medical decision-making, patient autonomy stands as a guiding principle, empowering individuals to take an active role in shaping their own healthcare journey. This concept is of paramount importance in the realm of genetic testing, where the potential implications of understanding one’s genetic makeup can profoundly impact future choices.
The Essence of Patient Autonomy
At the core of patient autonomy lies the belief that individuals possess the inherent right to make decisions about their own bodies and health. This principle recognizes that patients are not merely objects to be acted upon but rather active participants in their own care. By respecting their autonomy, healthcare professionals empower patients to take ownership of their health, fostering a sense of agency and well-being.
Empowering Patients in Genetic Testing
In the context of genetic testing, patient autonomy is particularly crucial due to the complex and potentially life-altering nature of the information that may be revealed. It is imperative that patients have access to comprehensive and understandable information about the potential benefits and risks of testing before they make informed choices.
Healthcare professionals have a duty to present patients with a clear and unbiased overview of the testing process, including its potential implications on their health, reproductive options, and family planning. Patients should have ample time to weigh the pros and cons and make a decision that aligns with their values and beliefs.
Balancing Autonomy and Responsibility
While respecting patient autonomy is paramount, it is also important to recognize that healthcare professionals have a responsibility to provide guidance and support to patients who may not have the necessary knowledge or experience to make fully informed decisions. This can involve sharing evidence-based information about the benefits and risks of testing, as well as exploring alternative options that may be available.
Patient autonomy is a fundamental pillar of ethical healthcare practice. By respecting the autonomy of patients in genetic testing, we not only empower them to make informed decisions about their own health but also preserve their dignity and human rights. Ultimately, it is through the recognition and preservation of patient autonomy that we truly honor the sacred bond between healthcare professional and patient.
Informed Consent: Empowering Patients in Genetic Testing
In the realm of healthcare, genetic testing plays a crucial role in unraveling the mysteries of our genetic makeup. However, with this powerful tool comes the ethical responsibility to ensure that patients are fully informed and give their consent before undergoing such procedures.
Informed consent requires that healthcare providers provide comprehensive and understandable information about the genetic testing process to their patients. This encompasses explaining the potential benefits and risks, the accuracy and limitations of the tests, and the implications of the results on their health and well-being.
Patients should be given ample opportunity to ask questions, voice concerns, and understand the ramifications of their choices. They should also be aware of the right to decline testing and the implications of doing so.
By respecting patient autonomy and providing transparent information, healthcare professionals can foster an atmosphere of trust and mutual understanding. This allows patients to make informed decisions that are aligned with their values and preferences.
Moreover, informed consent protects the rights of patients and ensures that they are treated with dignity and respect. It empowers them to take ownership of their healthcare journey and actively participate in shaping their medical decisions.
Remember, informed consent is not merely a legal obligation but an ethical imperative that empowers patients and ensures their well-being in the complex and ever-evolving field of genetic testing.
Unraveling the Secrets of Embryonic Development: Advancements in Genetic Research
In the intricate tapestry of life, genetic makeup plays a pivotal role, shaping who we are and how we develop. Ongoing research delves into the profound influence of genetics on the earliest stages of life – embryonic development. These groundbreaking efforts hold the potential to revolutionize our understanding and treatment of various medical conditions.
The Genetics of Embryonic Development
During embryonic development, the genetic material inherited from both parents intricately orchestrates the formation of tissues, organs, and systems. As the embryo grows, cell division and differentiation create a multitude of cell types, each with its unique function. Understanding the genetic mechanisms that govern these processes is paramount to comprehending normal development and the causes of birth defects.
Promises and Challenges in Genetic Research
Advances in genetic sequencing and analysis have provided scientists with unprecedented insights into the genetic basis of embryonic development. By studying the genomes of embryos and identifying specific genes and mutations associated with birth defects, researchers aim to shed light on the complex interactions that shape our health.
This knowledge has profound implications for advancing medical treatments. Researchers are exploring the possibility of using gene therapy to correct genetic mutations and prevent or mitigate birth defects. In addition, genetic screening can help identify couples at risk of having children with genetic conditions, allowing them to make informed reproductive decisions.
Ethical Considerations in the Pursuit of Knowledge
While the potential benefits of genetic research are immense, it also raises important ethical considerations. The complex nature of genetic information raises questions about privacy, confidentiality, and the potential for discrimination based on genetic data.
It is imperative to proceed with research in a responsible and ethical manner, ensuring that the benefits of genetic knowledge are balanced with the protection of individual rights. Informed consent and open dialogue are crucial to fostering public trust and ensuring that the fruits of genetic research are used for the betterment of society.
The frontiers of genetic research in embryonic development continue to expand, promising transformative advancements in the prevention, diagnosis, and treatment of birth defects. By unraveling the genetic mysteries that govern life’s earliest beginnings, we embark on a journey to empower individuals and improve the health outcomes of future generations.