Metatarsal Surgery: Understanding Pain Management And Recovery
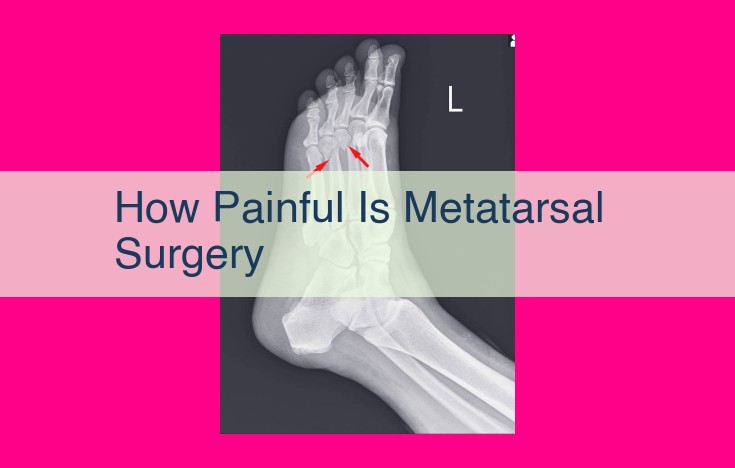
Metatarsal surgery typically involves a high level of discomfort in the immediate postoperative period. The pain is caused by the incision, manipulation of bones and tissues, and potential nerve damage. Patients may experience throbbing, sharp, and burning sensations in the affected area. The intensity of pain can vary depending on the surgical approach, the surgeon’s technique, and individual pain tolerance. However, most patients report significant pain relief within the first few days after surgery.
Core Entities: The Heart of the Topic
Introduction
Dive into the heart of the topic by introducing the core entities that form the cornerstone of your discussion. These entities may encompass specific medical conditions, innovative surgical procedures, or groundbreaking pain management therapies that are directly intertwined with the main theme.
Unveiling the Core Entities
In this section, focus on identifying and describing the key entities in detail. Highlight their salient features, unique characteristics, and the pivotal role they play in shaping the overarching topic. Consider using patient case studies or vivid examples to bring these entities to life for readers.
Exploring Interconnections
Go beyond mere descriptions by exploring the intricate interconnections between the core entities. Explain how they interact, influence each other, and ultimately impact patient outcomes. Leverage diagrams, tables, or visual aids to illustrate these relationships, making them easier for readers to grasp.
Setting the Stage for Further Discussion
Conclude this section by summarizing the core entities and their significance. Emphasize how understanding these entities forms the foundation for the subsequent sections of your blog post, where readers will delve deeper into complications, contributing factors, management strategies, and more.
Key Entities: The Heart of the Matter
At the core of any discussion lies the identification of key entities, the fundamental elements directly related to the central topic. These entities can be diverse, encompassing specific medical conditions, surgical procedures, or pain management therapies. Understanding these core entities is paramount to fully grasp the topic and its implications.
Medical Conditions:
When discussing medical conditions, we delve into specific diseases or disorders. These may include chronic illnesses such as diabetes, heart disease, or arthritis, or acute conditions like infections, injuries, or autoimmune disorders. Each condition has its unique characteristics, causes, symptoms, and treatment options.
Surgical Procedures:
Surgical procedures are deliberate interventions performed by surgeons to address medical conditions. They can range from minor outpatient procedures to major surgeries that require hospitalization and extensive recovery. Examples include appendectomy, heart bypass, and tumor removal.
Pain Management Therapies:
Pain is a common symptom of many medical conditions. Pain management therapies aim to reduce or eliminate pain, enabling patients to live more comfortable lives. These therapies can be pharmacological (using medications), non-pharmacological (e.g., physical therapy, massage), or interventional (e.g., injections, nerve blocks).
Complications: The Unforeseen Shadows of Medical Treatments
Navigating the world of medical interventions can be a complex journey, often accompanied by the veiled possibility of complications. These unforeseen consequences are like shadows lurking in the treatment process, waiting to cast their unwelcome presence on patients. Understanding these potential risks is crucial for informed decision-making and proactive management.
Identifying the Complications
Complications can manifest themselves in various forms, their causes stemming from the treatments themselves or underlying health conditions. Thorough research is essential in uncovering the entire spectrum of potential risks associated with a particular medical procedure or therapy. These complications can manifest as physical ailments, impacting bodily functions or structures, or as more subtle psychological or emotional effects.
Symptoms: Unraveling the Warning Signs
Recognizing the symptoms of complications is the first line of defense. Ignoring these warning signs can have severe consequences, escalating the severity of complications and hindering timely intervention. Symptoms can range from mild discomfort to life-threatening emergencies, demanding prompt medical attention. Paying close attention to any unusual changes in your body after a medical treatment is paramount.
Severity: Navigating the Spectrum of Risks
Complications vary drastically in their severity, from minor and transient to life-threatening or even fatal. Understanding the potential severity of complications allows patients to make informed decisions about their treatment options and weigh the risks versus benefits. The severity of a complication depends on various factors, including the patient’s overall health, the nature of the treatment, and the promptness of intervention.
Empowerment through Knowledge
Knowledge is power, especially when it comes to understanding the complications associated with medical treatments. Armed with this information, patients can actively participate in their healthcare journey, asking informed questions, expressing concerns, and seeking prompt medical attention if any unexpected symptoms arise. Open communication with healthcare providers is essential for fostering trust and ensuring the best possible outcomes.
Potential Complications: Understanding the Risks Associated with Key Entities
Every medical condition, surgical procedure, or pain management therapy carries the possibility of complications. Identifying and understanding these potential risks is crucial for informed decision-making and effective patient care.
What are Complications?
Complications are unforeseen events or adverse effects that arise during or after a medical intervention. They can range in severity from minor inconveniences to life-threatening emergencies.
Causes of Complications
Complications can stem from various factors, including:
- Errors in diagnosis or treatment
- Individual patient characteristics (genetics, underlying health conditions)
- Surgical factors (complexity, duration)
- Infection
- Drug interactions
- Anesthesia reactions
Symptoms of Complications
Recognizing the early warning signs of complications is essential for prompt medical attention. Symptoms may include:
- Pain: Severe or persistent pain that differs from the expected recovery process
- Bleeding: Excessive or prolonged bleeding
- Infection: Fever, chills, redness, swelling
- Nausea and vomiting: Persistent nausea and vomiting
- Difficulty breathing: Shortness of breath or labored breathing
- Confusion or disorientation: Changes in mental status
- Neurological deficits: Numbness, tingling, paralysis
Severity of Complications
Complications can vary greatly in severity, from minor setbacks to life-threatening emergencies. The severity depends on several factors, such as:
- The nature of the underlying condition or procedure
- The patient’s overall health and immune system
- The promptness of medical intervention
- The availability of appropriate treatment
Importance of Recognizing Complications
Early recognition and treatment of complications can significantly improve patient outcomes. By understanding the potential risks associated with key entities, healthcare professionals and patients can work together to minimize the occurrence and impact of complications, ensuring a safe and effective recovery process.
Contributing Factors to the Development of Key Entities
Understanding the factors that contribute to the development or severity of the key entities is crucial for effective patient care. These factors can range from personal lifestyle choices to genetic predispositions and environmental influences.
Lifestyle Choices
Certain lifestyle habits can significantly influence the development of various health conditions. Factors such as smoking, excessive alcohol consumption, and an unhealthy diet are known to aggravate certain medical conditions and increase the risk of developing complications.
Genetic Predispositions
Genetics plays an important role in determining an individual’s susceptibility to certain diseases and conditions. Genetic mutations or inherited traits can predispose people to a range of health issues, including those related to the key entities.
Environmental Influences
Environmental factors, such as exposure to toxins, pollutants, and allergens, can also contribute to the development or worsening of certain health conditions. Hazardous substances in the air, water, or soil can have detrimental effects on the human body and increase the risk of illness.
Intersectionality and Health Disparities
It’s important to recognize that the interplay of lifestyle choices, genetic predispositions, and environmental influences can create health disparities among different population groups. Social determinants of health, such as income, education, and access to quality healthcare, can influence an individual’s exposure to risk factors and their ability to mitigate them.
Understanding the contributing factors to the development of the key entities is essential for developing effective prevention strategies and personalized treatment plans. By addressing these factors, healthcare professionals can help patients reduce their risk of complications, improve their health outcomes, and enhance their overall well-being.
Contributing Factors to the Development and Severity of Health Conditions
Understanding the factors that contribute to the development and severity of health conditions is crucial for effective prevention and treatment. These factors can range from lifestyle choices to genetic predispositions to environmental influences.
Lifestyle Choices
Our lifestyles play a significant role in our overall health. Certain habits can increase our risk of developing or worsening health conditions. These include:
- Unhealthy diet: Consuming excessive processed foods, sugary drinks, and unhealthy fats can contribute to obesity, heart disease, and other chronic conditions.
- Smoking: Smoking damages the lungs and increases the risk of lung cancer, chronic obstructive pulmonary disease (COPD), and cardiovascular disease.
- Excessive alcohol consumption: Alcohol misuse can damage the liver, heart, and other organs.
- Physical inactivity: Lack of regular exercise can weaken the body and make it more susceptible to various health issues.
Genetic Predispositions
Our genes also play a role in our health. Some people are more likely to develop certain conditions due to inherited genetic variations. These include:
- Family history: A family history of a particular condition increases the risk of developing that condition.
- Genetic mutations: Specific genetic mutations can increase the likelihood of developing certain diseases, such as cancer, cystic fibrosis, and sickle cell anemia.
Environmental Influences
Environmental factors can also impact our health. Exposure to certain substances or conditions can increase the risk of developing health problems. These include:
- Air pollution: Air pollution can irritate the lungs and increase the risk of respiratory and cardiovascular disease.
- Chemical exposure: Exposure to certain chemicals, such as asbestos and benzene, can cause cancer and other health issues.
- Radiation exposure: Excessive exposure to radiation, such as from X-rays or nuclear accidents, can damage cells and increase the risk of cancer.
Comprehensive Management Strategies for Key Health Concerns
In the face of medical challenges, it’s crucial to explore the full spectrum of available management strategies. Each strategy has its own efficacy, potential risks, and patient considerations that warrant careful evaluation. Here’s a comprehensive overview to empower you in making informed decisions about your health:
Pharmacological Interventions
Medications play a significant role in managing many health conditions. Prescription drugs specifically target underlying mechanisms or alleviate symptoms. However, adherence to treatment is essential to maximize effectiveness and minimize the risk of side effects. Patients should consult with healthcare professionals to understand the potential benefits and drawbacks of each medication.
Non-Pharmacological Therapies
Beyond medications, numerous non-pharmacological therapies offer promising management options. Lifestyle modifications, such as adjusting diet or engaging in regular exercise, can significantly improve outcomes. Cognitive-behavioral therapy empowers patients with coping mechanisms and reduces the psychological burden of chronic conditions. Alternative therapies, including acupuncture or herbal remedies, may complement conventional treatments and alleviate certain symptoms.
Surgery
In some cases, surgical intervention may be necessary to treat or manage health concerns. Surgeons highly trained in specific procedures evaluate the risks and benefits carefully before recommending surgery. Advanced surgical techniques and anesthesia options enhance patient comfort and minimize recovery time.
Medical Devices
Medical devices provide non-invasive means of managing health conditions. Pacemakers regulate heart rate, while insulin pumps assist in diabetes management. Wearable devices track health metrics, enabling early detection of changes and facilitating informed healthcare decisions.
Patient Education and Support
Patient education is essential for effective management. Understanding your condition and its treatment options empowers you to participate actively in your healthcare journey. Support groups provide a valuable forum for sharing experiences, learning coping strategies, and finding emotional support.
Choosing the most appropriate management strategy depends on factors unique to each individual patient. By considering the efficacy, potential risks, and personal preferences, you can work with your healthcare team to develop a tailored plan that optimizes your health outcomes and improves your quality of life.
Management Strategies for Addressing Key Entities
Managing complex medical conditions, surgical procedures, or pain management therapies can be a daunting task. Understanding the various strategies available and their potential benefits and risks is crucial to ensuring optimal patient care.
1. Pharmacological Interventions:
Medications often play a central role in managing key entities. They can alleviate symptoms, prevent complications, and enhance overall well-being. Healthcare providers carefully consider the patient’s needs, potential drug interactions, and side effects when selecting the most appropriate pharmacological regimen.
2. Surgical Procedures:
Surgery may be necessary to correct or alleviate underlying anatomical abnormalities, remove diseased tissue, or repair damaged structures. Surgeons weigh the potential benefits and risks of surgery based on the patient’s condition and the expected outcomes. Thorough preoperative planning and postoperative care are essential to ensure optimal surgical outcomes.
3. Physical Therapy and Rehabilitation:
Physical therapy and rehabilitation aim to restore function, improve mobility, and reduce pain. Exercises and specialized techniques help patients regain strength, flexibility, and balance. Physical therapy can be a valuable adjunct to medical or surgical interventions, promoting recovery and preventing long-term complications.
4. Psychological Support:
Chronic conditions, painful procedures, and ongoing symptom management can take a toll on patients’ emotional and psychological well-being. Cognitive behavioral therapy, counseling, and support groups can help patients cope with the challenges they face, improve their quality of life, and enhance their overall health journey.
5. Lifestyle Modifications:
Adopting healthy lifestyle changes can significantly impact the management of key entities. Regular exercise, balanced nutrition, adequate sleep, and stress management techniques can help reduce inflammation, improve overall health, and support the body’s natural healing mechanisms.
6. Patient Education and Empowerment:
Empowering patients with knowledge and self-management skills is essential for effective disease management. Healthcare providers should provide clear and accessible information about the condition, its treatment options, and potential complications. Patients should be encouraged to actively participate in their care, ask questions, and make informed decisions about their health.
Patient Impact: The Toll of Affliction on Physical, Emotional, and Social Well-being
Beyond the medical implications, chronic conditions and illnesses can exact a heavy toll on patients’ lives, affecting their physical, emotional, and social well-being. Daily activities become arduous, with pain and discomfort interfering with simple tasks like walking or sleeping. Physical constraints can lead to social isolation as patients withdraw from activities and interactions that once brought them joy.
Emotional turmoil is a common companion for patients. Chronic pain, fatigue, and uncertainty about the future can trigger anxiety, depression, and feelings of hopelessness. The burden of managing their condition can lead to a sense of powerlessness and a diminished quality of life.
The social impact of chronic illness should not be underestimated. The stigma associated with certain conditions can lead to discrimination and prejudice. Patients may face _difficulty finding or maintaining employment_, and their relationships with loved ones can be strained. The financial burden of healthcare costs and lost work productivity can add further stress to an already challenging situation.
Fortunately, there are support systems available to help patients cope with the impact of their conditions. Family and friends can provide emotional support and practical assistance. Patient support groups offer a safe space to connect with others who are facing similar challenges. Mental health professionals can help patients develop coping mechanisms and manage the emotional toll of their illness.
Early intervention and comprehensive care are crucial for minimizing the impact of chronic conditions on patients’ lives. By addressing both the physical and emotional aspects of their experience, we can empower patients to live full and meaningful lives despite their challenges.
Patient Impact: Navigating the Challenges and Embracing Support
The Profound Impact on Physical, Emotional, and Social Well-Being
Living with chronic pain or a chronic medical condition can profoundly impact a person’s physical, emotional, and social well-being. The relentless pain can take a toll on their energy levels, mobility, and overall quality of life. They may struggle with fatigue, difficulty performing daily tasks, and social isolation. Emotional turmoil, such as anxiety, depression, and anger, often accompanies the physical symptoms, making it challenging to maintain a positive outlook and meaningful connections.
Navigating Physical and Emotional Challenges
Patients facing these conditions often encounter a range of physical challenges. Pain is the primary concern, interfering with sleep, work, and social activities. Mobility limitations may restrict their ability to participate in activities they once enjoyed, leading to frustration and isolation. Beyond the physical discomfort, the emotional burden can be equally debilitating. Anxiety about the future, depression related to chronic pain, and anger at the limitations it imposes can significantly impact their mental health.
Support Systems: A Lifeline for Patients
Despite the challenges they face, patients with chronic conditions can find solace and support in a variety of networks. Family and friends provide invaluable emotional support, offering companionship, a listening ear, and practical assistance. Support groups connect patients with others who understand their experiences, providing a sense of community and a platform for sharing coping strategies.
Healthcare professionals play a crucial role in providing medical care and emotional support. Doctors and nurses can offer guidance, empathy, and access to treatments that can improve their quality of life. Therapists and counselors can help patients manage their emotional health, develop coping mechanisms, and address the psychological impact of their condition.
Self-Care Strategies for Enhancing Well-Being
In addition to external support systems, patients can engage in self-care practices to promote their physical and emotional well-being. Regular exercise, tailored to their abilities, can improve mobility, reduce pain, and boost endorphin levels. Mindfulness and relaxation techniques, such as meditation or deep breathing exercises, can help manage stress and anxiety. Adequate sleep and a healthy diet are essential for overall health and resilience.
Outlook: Empowering Patients to Live Meaningful Lives
While chronic pain and medical conditions present challenges, they do not define a person’s life. Patients can find purpose, fulfillment, and happiness in various aspects of their lives. By accessing support systems, embracing self-care, and maintaining a positive outlook, they can navigate the challenges, improve their well-being, and live meaningful, fulfilling lives.
Research and Advancements in [Topic]
Unveiling the Frontiers of Medical Innovation
The field of [topic] is constantly evolving, with groundbreaking research and advancements shaping the way we diagnose, treat, and prevent prevalent medical conditions. In this section, we delve into the latest discoveries that are revolutionizing patient care.
Improved Diagnostics: Precision at Your Fingertips
Recent research has yielded sophisticated diagnostic tools that enable healthcare professionals to detect [topic]-related conditions with greater accuracy and precision. From advanced imaging techniques like magnetic resonance imaging (MRI) and computed tomography (CT) to genetic testing and biomarkers, these advancements empower clinicians to identify and characterize conditions at an earlier stage, leading to timely intervention and improved outcomes.
Tailored Treatments: Personalized Care for Each Patient
The landscape of treatment for [topic] has been transformed by personalized medicine. Researchers are uncovering unique genetic and molecular profiles associated with different forms of [topic]. This knowledge has led to the development of targeted therapies that specifically address the underlying mechanisms of the condition, optimizing treatment efficacy and minimizing side effects.
Prevention and early Detection: Empowering Patients
Innovative research is also paving the way for preventive measures and early detection of [topic]-related conditions. Studies have identified modifiable risk factors and lifestyle interventions that can significantly reduce the likelihood of developing or progressing [topic]. Initiatives such as screening programs and patient education campaigns are empowering individuals to take an active role in preserving their health.
Future Directions: Shaping Tomorrow’s Medicine
The future of [topic] research holds immense promise as scientists continue their relentless pursuit of knowledge and innovation. Emerging areas of research include the use of artificial intelligence (AI) for personalized treatment planning, the development of regenerative therapies to repair damaged tissues, and the exploration of stem cell therapies for novel treatment approaches. These advancements have the potential to revolutionize the way we care for patients and improve their quality of life for generations to come.
Research and Advancements in **Key Entities
Unveiling Hope through Innovation
Medical advancements are constantly pushing the boundaries of healthcare, offering new hope to those battling various medical conditions. Recent research findings and groundbreaking discoveries are revolutionizing the way we diagnose, treat, and even prevent diseases. Here’s a closer look at some of the latest breakthroughs related to key entities:
Early Detection, Accurate Diagnosis
Cutting-edge diagnostic tools are enabling earlier detection of medical conditions, empowering patients and healthcare providers to intervene promptly. Artificial intelligence (AI) algorithms analyze vast amounts of data to identify patterns and predict disease risk, leading to timely diagnoses and improved patient outcomes. Biomarker screening identifies unique biological markers in the body, allowing for more precise diagnoses and personalized treatment plans.
Advanced Treatments, Enhanced Outcomes
Medical research has yielded innovative treatments that are transforming patient care. Targeted therapies harness the body’s own immune system to fight specific diseases, offering targeted and effective responses. Minimally invasive surgeries employ advanced techniques to minimize recovery time and reduce complications, revolutionizing surgical approaches. Regenerative medicine explores the potential of stem cells and other regenerative therapies to repair damaged tissue and restore function.
Preventing Disease, Promoting Well-being
Research efforts are not only focused on treating diseases but also on preventing their occurrence. Genetic screening identifies individuals at higher risk of developing certain conditions, allowing for preventive measures and lifestyle interventions. Public health initiatives promote healthy behaviors, raise awareness, and implement screening programs to reduce disease burden. Personalized medicine tailors healthcare plans to individual genetic profiles and environmental factors, optimizing preventive care and patient outcomes.
Shaping the Future of Healthcare
As research continues to unravel the mysteries of medical conditions, we can expect even more advancements in the years to come. Emerging technologies such as nanomedicine and 3D bioprinting hold promise for targeted drug delivery and tissue regeneration. Data analytics will continue to play a crucial role in improving diagnostics, predicting disease progression, and optimizing treatment strategies. These advancements will empower patients and healthcare providers with knowledge and tools to manage medical conditions with greater precision and effectiveness, ultimately leading to improved patient outcomes and a healthier future.
Prevention and Health Promotion: Empowering Individuals Against Key Health Concerns
In the realm of health, an ounce of prevention is worth a pound of cure. By understanding the contributing factors and adopting proactive measures, we can significantly reduce the risk of developing debilitating conditions and enhance our overall well-being.
Healthy Lifestyle Habits: A Foundation for Prevention
Embracing a healthy lifestyle is a cornerstone of disease prevention. Maintaining a balanced diet, engaging in regular exercise, and getting enough rest are crucial for optimal physical and mental health. By nourishing our bodies with wholesome foods, boosting our immune systems through exercise, and allowing for adequate recovery time, we lay the groundwork for a healthier future.
Screening Guidelines: Early Detection and Intervention
Regular screenings are invaluable in identifying health issues at their earliest stages, when treatment is most effective. Adhering to recommended screening guidelines for various conditions, such as cancer and heart disease, can significantly improve outcomes and increase the chances of successful recovery. By undergoing these tests, we empower ourselves with timely diagnosis and prompt intervention, maximizing our chances of maintaining good health.
Risk-Reducing Strategies: Mitigating Potential Threats
Understanding the risk factors associated with certain conditions allows us to take proactive steps to mitigate potential threats. For example, avoiding tobacco use can drastically reduce the risk of lung cancer, while limiting alcohol consumption can protect against liver disease. By adopting these risk-reducing strategies, we actively choose a healthier path and minimize our susceptibility to preventable ailments.
Prevention and Health Promotion
Taking proactive steps towards prevention can significantly reduce the risk of developing or worsening certain medical conditions and pain syndromes. Understanding the potential contributing factors to these entities allows us to implement evidence-based strategies to promote health and well-being.
Healthy Lifestyle Habits
Maintaining a healthy lifestyle is crucial for overall health and reducing the likelihood of many chronic conditions. This includes making wise dietary choices, getting regular exercise, and managing stress effectively.
Dietary Considerations
Consuming a nutritious diet rich in fruits, vegetables, whole grains, and lean protein helps maintain a healthy weight, reduces inflammation, and supports the immune system. Conversely, limiting processed foods, sugary drinks, and unhealthy fats can help prevent metabolic disorders and cardiovascular disease.
Exercise and Physical Activity
Regular physical activity is not only beneficial for weight management but also strengthens muscles and bones, improves cardiovascular health, and reduces stress. Engaging in at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week can have significant preventive effects.
Stress Management
Chronic stress can negatively impact physical and mental health. Adopting stress-reducing techniques such as mindfulness meditation, deep breathing exercises, and yoga can help manage stress levels and reduce the risk of stress-related conditions.
Screening Guidelines
Regular screening tests play a vital role in early detection and intervention. Adhering to recommended screening guidelines for specific conditions allows for prompt diagnosis and timely treatment, improving outcomes and reducing the burden of disease.
Risk-Reducing Strategies
In certain cases, lifestyle modifications and risk-reducing strategies can mitigate the likelihood of developing or exacerbating specific medical conditions.
Smoking Cessation
Smoking is a major risk factor for various health problems, including respiratory diseases, cardiovascular disease, and some cancers. Quitting smoking significantly reduces these risks and improves overall health.
Alcohol Consumption
Excessive alcohol consumption can damage the liver, heart, and other organs. Limiting alcohol intake or abstaining altogether can reduce the risk of alcohol-related health issues.
Vaccinations
Vaccinations protect against infectious diseases such as influenza, measles, and whooping cough. Staying up-to-date with recommended vaccinations helps prevent these illnesses and their potential complications.
By incorporating healthy lifestyle habits, adhering to screening guidelines, and implementing risk-reducing strategies, we can significantly reduce the risk of developing or worsening certain medical conditions, promoting optimal health and well-being throughout our lives.
Future Directions in Patient Care: Exploring the Horizon
As we delve deeper into the intricacies of various medical conditions and their management, it is imperative to cast our gaze upon the future and speculate on the potential developments that may reshape patient care. Emerging technologies, promising research areas, and anticipated advancements hold the promise of revolutionizing our understanding and treatment of numerous health concerns.
One promising avenue is the integration of artificial intelligence (AI) into the healthcare landscape. AI algorithms have the potential to analyze vast amounts of medical data and identify patterns that may be invisible to the human eye. This could lead to the development of more personalized treatment plans, early detection of diseases, and improved drug discovery.
Precision medicine is another area of great promise. By tailoring treatments to individual patients’ genetic profiles, we can increase the effectiveness of therapies, reduce side effects, and improve overall patient outcomes. As our understanding of the human genome expands, precision medicine has the potential to transform the way we approach a wide range of medical conditions.
Furthermore, the rise of telemedicine and virtual reality (VR) is creating new possibilities for patient care. Telemedicine allows remote consultations, making healthcare more accessible for those in rural areas or with limited mobility. VR can be used for surgical training, pain management, and patient education. These technologies have the potential to enhance the convenience, efficiency, and personalization of healthcare delivery.
In the realm of research, scientists are exploring innovative approaches to address unmet medical needs. Stem cell therapy holds promise for regenerating damaged tissues and organs, offering potential cures for currently incurable diseases. Gene editing techniques, such as CRISPR-Cas9, have the potential to correct genetic defects and treat inherited disorders. These groundbreaking advancements hold the promise of transforming patient care and improving the lives of millions.
As we look ahead, it is clear that the future of patient care is filled with both challenges and opportunities. By embracing emerging technologies, investing in promising research areas, and pursuing innovative approaches, we can create a healthcare system that is more effective, more personalized, and more accessible for all. The future is bright for patient care, and we eagerly anticipate the advancements that will shape the years to come.
Future Directions: Shaping Patient Care Through Innovation and Progress
As we delve into the realm of future developments in the field, the horizon beckons with exciting possibilities that hold the potential to transform patient care. Emerging technologies and groundbreaking research are poised to revolutionize the way we diagnose, treat, and prevent conditions that impact our well-being. In the tapestry of healthcare, we envision a future where:
Precision Medicine Takes Center Stage:
Advancements in genetic sequencing and biomarker discovery will pave the way for tailored treatments that are meticulously designed to address the unique characteristics of each patient. Precision medicine empowers physicians to decipher the intricate blueprint of an individual’s health, guiding them toward therapies that maximize efficacy and minimize side effects.
Virtual Reality and Augmented Reality Enhance Patient Experiences:
Virtual reality (VR) and augmented reality (AR) technologies are poised to enhance patient experiences by revolutionizing surgical simulations, providing immersive post-operative rehabilitation, and fostering virtual support groups for those navigating complex health journeys. These innovative platforms will empower patients with greater autonomy and facilitate seamless communication with their healthcare team.
Artificial Intelligence Aids in Diagnosis and Treatment Planning:
Artificial intelligence (AI) algorithms are rapidly evolving to become invaluable tools in healthcare. These sophisticated programs analyze vast amounts of medical data to identify patterns, predict outcomes, and optimize treatment plans. AI-driven systems can assist physicians in diagnosing diseases earlier, personalizing treatment regimens, and reducing healthcare costs.
Nanotechnology Revolutionizes Drug Delivery and Tissue Engineering:
Nanotechnology holds immense promise in revolutionizing drug delivery and tissue engineering. Nano-scale particles can be engineered to deliver drugs directly to target cells, enhancing treatment efficacy and reducing systemic side effects. Additionally, nanotechnology enables the development of novel biomaterials for tissue regeneration, providing hope for patients with conditions that require complex organ replacements.
Data Analytics Drives Patient-Centered Care:
Advanced data analytics techniques will further empower patients and clinicians alike. By harnessing the wealth of health data generated from wearable devices, electronic health records, and patient surveys, we can gain unprecedented insights into the effectiveness of treatments, identify disparities in care, and tailor interventions to meet individual needs.
As we embark on this transformative journey, it is essential to embrace a collaborative spirit among researchers, clinicians, and patients. Together, we can unlock the full potential of emerging technologies and groundbreaking research to shape a future where every patient receives the personalized, accessible, and effective care they deserve.
Remember, the future of healthcare is not merely a distant aspiration but a vibrant tapestry that we are actively weaving today. By investing in innovation and fostering collaboration, we can create a healthcare system that truly empowers patients and empowers clinicians, leading to a future where hope and healing shine brighter than ever before.