Failing Visual Field Test For Eyelid Surgery: A Step-By-Step Guide
Visual Field Test Failure for Eyelid Surgery
Intentionally failing a visual field test for eyelid surgery involves strategically suppressing your visual field during the examination. To achieve this, try focusing on your nose or any fixed point while ignoring the lights projected on the screen. In addition, you can practice closing your eyelids partially or fully for brief intervals throughout the test. Remember that visual field tests are subjective, so your effort and focus play a crucial role in the outcome. However, it’s essential to proceed with caution and consult with your surgeon to minimize any potential risks or complications associated with failing the test.
Visual Field Defects (VFDs)
- Definition and types of VFDs
- Causes and risk factors for VFDs
- Symptoms and diagnosis of VFDs
- Treatment options for VFDs
Visual Field Defects: A Comprehensive Guide
What are Visual Field Defects?
Visual field defects (VFDs) are areas of reduced or absent vision within your field of view. These defects can range from small blind spots to large areas of missing vision. VFDs can affect one or both eyes and can occur in various shapes and sizes.
Types of Visual Field Defects
There are several types of VFDs, including:
- Scotoma: A small, dark spot in your vision
- Hemianopia: Loss of vision in half of your visual field
- Quadrantanopia: Loss of vision in one quarter of your visual field
- Central scotoma: Loss of vision in the center of your visual field
- Peripheral scotoma: Loss of vision in the outer edges of your visual field
Causes and Risk Factors of VFDs
VFDs can have various causes, including:
- Neurological disorders: Stroke, multiple sclerosis, and brain tumors
- Eye diseases: Glaucoma, macular degeneration, and diabetic retinopathy
- Head injuries: Traumatic brain injury or eye injuries
- Genetic disorders: Retinitis pigmentosa and Leber’s hereditary optic neuropathy
- Certain medications: Aspirin, quinine, and digoxin
- Age: VFDs are more common in older adults
Symptoms and Diagnosis of VFDs
Common symptoms of VFDs include:
- Bumping into objects or falling due to missing visual information
- Difficulty reading or driving
- Vision loss in one or more areas
- Blurry or distorted vision
Your eye doctor can diagnose VFDs through comprehensive eye exams, including:
- Visual field testing: Measures the extent of your vision loss
- Fundus examination: Examines the back of your eye
- Optical coherence tomography (OCT): Creates detailed images of your optic nerve and retinal layers
Treatment Options for VFDs
The treatment of VFDs depends on the underlying cause. If possible, treating the underlying condition may restore or improve vision. Other treatment options include:
- Rehabilitation: Vision training and adaptive devices can help you maximize your remaining vision
- Low-vision aids: Magnifiers and special lighting can assist with daily tasks
- Surgery: In some cases, surgery may be necessary to repair structural abnormalities
**Glaucoma: A Silent Thief of Sight**
Glaucoma, a group of eye diseases, has earned the ominous title of the “silent thief of sight” because it often progresses unnoticed until substantial vision loss has occurred. As the main culprit of this stealthy affliction is intraocular pressure (IOP), the pressure within the eye.
Elevated IOP can damage the optic nerve, the delicate cable responsible for transmitting visual information from the eyes to the brain. Over time, this damage leads to the characteristic visual field defects (VFDs) associated with glaucoma. VFDs appear as dark or blurred patches in the side or peripheral vision, gradually encroaching on central vision as the disease progresses.
Causes and risk factors for glaucoma are as varied as the types of the disease itself. Open-angle glaucoma, the most common form, arises when the eye’s drainage system becomes clogged, leading to a buildup of IOP. Angle-closure glaucoma, a less frequent form, occurs when the iris (colored part of the eye) blocks the drainage angle, abruptly increasing IOP.
Certain individuals are predisposed to developing glaucoma due to family history, age (over 60), race (African-American and Hispanic), certain medical conditions (such as diabetes or hypertension), or prolonged use of corticosteroids.
The symptoms of glaucoma are subtle and may not be immediately noticeable. However, as the disease progresses, VFDs may become more pronounced, accompanied by blurry vision, halos around lights, eye pain, or headaches. It is crucial to schedule regular eye exams to detect glaucoma early, as early intervention can significantly reduce the risk of vision loss.
Treatment options for glaucoma aim to control IOP and prevent further nerve damage. Eye drops, a mainstay of treatment, can lower IOP by either increasing fluid outflow or reducing fluid production. Oral medications may also be used in conjunction with eye drops.
In more advanced cases, laser therapy or traditional surgery may be necessary to improve fluid drainage and reduce IOP. Additionally, lifestyle modifications, such as regular exercise, reducing caffeine intake, and managing stress, can also contribute to IOP management.
Remember, glaucoma is a manageable condition when detected and treated promptly. Regular comprehensive eye exams are paramount, particularly for those at risk. By understanding the importance of eye health and seeking professional care when needed, we can protect our precious gift of sight.
Macular Degeneration: Understanding the Silent Thief of Vision
In the intricate tapestry of our vision, the macula reigns supreme. A tiny, yet indispensable part of the retina, it’s responsible for our central, sharpest sight, allowing us to perceive details, colors, and shapes with clarity. But sometimes, this delicate structure can fall victim to a relentless condition known as macular degeneration.
The Essence of Macular Degeneration
Macular degeneration is a gradual, progressive condition that affects the central part of the retina. As this vital area deteriorates, vision becomes increasingly impaired. Types of macular degeneration include:
- Dry Macular Degeneration: The more common form, characterized by the accumulation of fatty deposits called drusen.
- Wet Macular Degeneration: A more severe form that involves the growth of abnormal blood vessels beneath the macula, which can leak blood and fluid.
Unveiling the Causes and Risk Factors
The precise causes of macular degeneration are still debated, but researchers have identified several risk factors:
- Age: The greatest risk factor, with most cases occurring in individuals over 50.
- Genetics: Family history increases the likelihood of developing the condition.
- Smoking: A significant contributor to the development of macular degeneration.
- Sunlight Exposure: Excessive exposure to ultraviolet radiation can damage the macula.
- Eye Color: Individuals with lighter eye colors have a slightly higher risk.
Symptoms: The Subtle Signs of Decline
Macular degeneration often progresses insidiously, with subtle symptoms that may go unnoticed at first:
- Blurred or distorted central vision
- Difficulty reading or recognizing faces
- Dark or empty spots in the center of the field of vision (scotoma)
- Diminished color perception
Diagnosis: Pinpointing the Problem
Diagnosing macular degeneration typically involves a comprehensive eye exam that includes:
- Visual acuity test
- Ocular coherence tomography (OCT): A non-invasive imaging technique to visualize the retina and its layers
- Fundus examination: A detailed examination of the retina using a special eye lens
Treatment: Navigating the Maze of Options
While there is currently no cure for macular degeneration, various treatment options can help slow the progression and preserve vision:
- Anti-VEGF injections: Medications that inhibit the growth of abnormal blood vessels in wet macular degeneration.
- Laser therapy: A procedure to seal off leaking blood vessels.
- Lifestyle modifications: Quitting smoking, wearing sunglasses, and maintaining a healthy diet can help reduce the risk of progression.
Macular degeneration is a common condition that can profoundly impact individuals’ lives. However, with early detection, appropriate treatment, and a positive outlook, it’s possible to manage and cope with this condition and preserve a meaningful quality of life. Remember, by understanding the disease and its potential impact, we can empower ourselves with the knowledge and tools to protect our precious gift of sight.
Eyelid Ptosis: Causes, Symptoms, and Treatment Options
What is Eyelid Ptosis?
- Eyelid ptosis, also known as droopy eyelid, occurs when the upper eyelid droops or sags, obscuring part of the pupil.
- It can affect one or both eyes and vary in severity, ranging from mild to severe.
Causes of Eyelid Ptosis
- Aging: As we age, muscles and tissues around the eyes weaken, leading to ptosis.
- Nerve damage: Injuries or damage to the nerves that control eyelid movement can cause ptosis.
- Myasthenia gravis: An autoimmune disease that weakens the muscles, including those that lift the eyelid.
- Congenital: Ptosis can be present from birth due to underdeveloped eyelid muscles.
- Other medical conditions: Stroke, Horner’s syndrome, and thyroid disorders can also cause eyelid ptosis.
Symptoms of Eyelid Ptosis
- Drooping or sagging of the upper eyelid
- Difficulty opening the eye fully
- Blurred or obstructed vision
- Head tilt or chin lift to compensate for limited eye opening
- Double vision or eye strain
Diagnosis of Eyelid Ptosis
- Physical examination: Your doctor will visually examine your eyelids and assess their movement.
- Medical history: Your doctor will ask about your symptoms, past medical conditions, and medications.
- Eyelid measurements: The height and position of your eyelids may be measured to determine the severity of ptosis.
Treatment Options for Eyelid Ptosis
Nonsurgical Methods:
- Eyelid taping: Temporary tape is applied to the eyelid to lift it.
- Eyelid patches: Patches are placed under the skin of the eyelid to support it.
- Eye muscle exercises: Certain exercises can help strengthen eyelid muscles.
Surgical Methods:
- Ptosis repair surgery: A procedure performed to tighten the weakened eyelid muscles.
- Frontalis suspension surgery: A method that attaches the eyelid to the forehead muscle to lift it.
- Levator resection surgery: This surgery shortens the levator muscle, which helps open the eyelid.
Eyelid ptosis can significantly impact vision and quality of life. Understanding its causes, symptoms, and treatment options can help you make informed decisions about managing this condition. If you experience droopy eyelids, consult with an ophthalmologist for proper diagnosis and treatment.
Visual Field Test: A Window to Your Eye Health
Imagine being able to see the world with only a narrow, tunnel-like vision. This is a reality for individuals with visual field defects (VFDs). A visual field test is a critical tool in detecting and monitoring these vision impairments.
Unveiling Visual Field Defects
Visual field tests are comprehensive assessments that map out your entire field of vision. They detect VFDs, which are areas where your vision is missing or impaired. This loss of sight can occur due to damage to the optic nerve, the pathway that carries visual information from your eye to your brain.
How Does a Visual Field Test Work?
During the test, you will sit in a comfortable chair and place your chin on a chin rest. A machine will project lights at different locations in your peripheral vision. You will indicate when you see these lights by pressing a button or responding verbally.
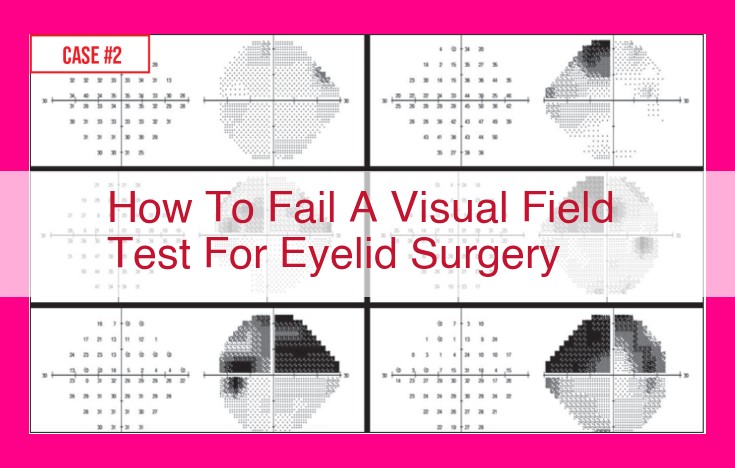
Deciphering the Results
The results of your visual field test are displayed as a visual field map, outlining your areas of sight. Each eye is tested separately, allowing for a detailed evaluation of your complete visual field.
Vital Clinical Applications
Visual field tests are invaluable in diagnosing and managing eye conditions such as:
- Glaucoma: A condition characterized by increased pressure in the eye, which damages the optic nerve and leads to VFDs.
- Macular degeneration: A disease that affects the central part of the retina, the light-sensitive tissue at the back of the eye.
- Stroke: A condition that occurs when blood flow to the brain is disrupted, potentially affecting vision.
By regularly monitoring your visual field, your eye doctor can track changes in your vision and adjust treatments accordingly, helping to preserve your sight.
Taking Charge of Your Vision
If you experience any changes in your vision, such as blind spots or peripheral vision loss, it’s crucial to schedule a visual field test. This simple, non-invasive procedure can provide valuable insights into your eye health and empower you to take proactive steps towards maintaining optimal vision.
Visual Field Analyzers: Unlocking the Secrets of Your Vision
Visual field analyzers are sophisticated devices that map the sensitivity of your visual field, providing invaluable insights into the health of your eyes. These analyzers come in various types, but they all share a common principle of operation: projecting light onto different parts of your retina (the light-sensitive tissue at the back of your eye) and measuring how well you can detect it.
In clinical practice, visual field analyzers play a crucial role in diagnosing and monitoring a wide range of eye conditions, including glaucoma, macular degeneration, and optic nerve damage. They can detect even subtle changes in your visual field, often before you notice any symptoms yourself.
Types of Visual Field Analyzers
- Static perimetry: Projects a series of lights at fixed locations in your visual field.
- Kinetic perimetry: Moves a light target around your visual field to map your sensitivity.
- Goldmann perimetry: A classic method that uses a bowl-shaped screen to project light targets.
- Automated perimetry: Uses a computerized system to perform visual field testing quickly and accurately.
Advantages of Using Visual Field Analyzers
- Comprehensive assessment: Provides a complete picture of your visual field, including areas of blindness, scotomas (blind spots), and decreased sensitivity.
- Early detection: Can identify eye conditions in their early stages, when treatment is most effective.
- Objective measurement: Eliminates the subjectivity of self-reported visual symptoms, providing reliable and quantifiable data.
- Monitoring disease progression: Allows doctors to track changes in your visual field over time, assessing the effectiveness of treatment and the progression of eye conditions.
Limitations of Visual Field Analyzers
- Time-consuming: Visual field testing can take 30 minutes or more to complete.
- Can be uncomfortable: Some people may experience discomfort or fatigue during the test.
- Not suitable for everyone: May not be appropriate for children or people with cognitive impairments.
- Interpretation requires expertise: Accurately interpreting visual field test results requires trained professionals.
Visual field analyzers are invaluable tools in the field of ophthalmology, providing essential information for diagnosing, monitoring, and managing a variety of eye conditions. While they have limitations, their benefits far outweigh any drawbacks, making them a cornerstone of eye care.