Assess And Manage Fluid Status: Identifying And Addressing Euvolemia And Dehydration
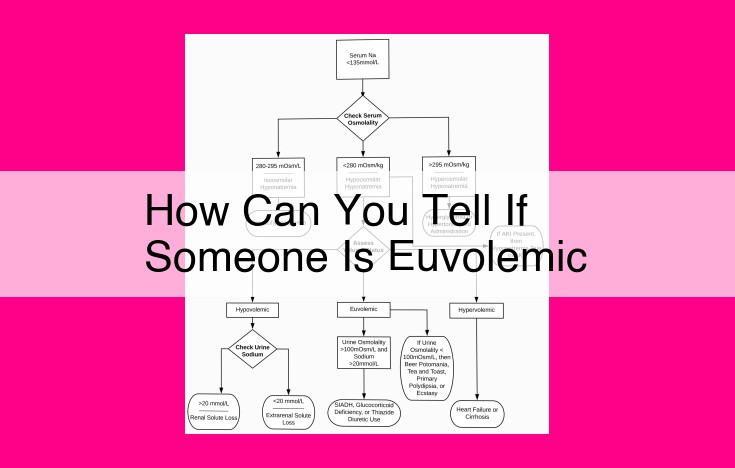
To determine if someone is euvolemic, assess clinical signs such as blood pressure, heart rate, and lung auscultation. Biochemical markers like serum sodium, potassium, and creatinine can indicate dehydration severity. Additionally, consider symptoms like dehydration or overhydration, mental status, oral fluid tolerance, and electrolyte balance. Promptly address dehydration, especially in vulnerable populations, as untreated dehydration can lead to complications. Encourage prevention by staying hydrated, consuming electrolyte-rich foods, and seeking medical attention when symptoms persist.
Clinical Assessment of Dehydration: Recognizing Signs and Taking Action
Dehydration occurs when the body loses more fluids than it takes in, leading to a water and electrolyte imbalance. While mild dehydration is common and usually easily remedied, severe dehydration can be life-threatening, especially for vulnerable populations like children and the elderly. Therefore, it’s crucial to recognize the clinical signs of dehydration and take prompt action.
Physical Examination
The first step in assessing dehydration is a thorough physical examination. Dehydrated individuals may exhibit various clinical signs, including:
-
Low blood pressure (hypotension): Dehydration reduces blood volume, leading to a decrease in blood pressure.
-
Elevated heart rate (tachycardia): The heart pumps faster to compensate for decreased blood volume.
-
Dry mucous membranes in the mouth, nose, and eyes indicate a loss of fluids.
-
Decreased skin turgor, or the skin’s elasticity, is a sign of dehydration. When pinched, dehydrated skin slowly returns to its original position.
-
Sunken eyes: Dehydration causes the eyes to appear sunken or “hollowed out.”
-
Rapid or shallow breathing: Dehydration can lead to respiratory distress.
Auscultation of Lungs
Auscultation of the lungs can also provide clues to dehydration. Dehydrated individuals may have:
-
Dry or crackling lung sounds (rales): These sounds indicate fluid loss from the alveoli, the tiny air sacs in the lungs.
-
Decreased or absent breath sounds: Severe dehydration can lead to reduced lung function.
Importance of Recognizing Signs
Recognizing the clinical signs of dehydration is essential to prevent serious complications. Prompt action should be taken if any of these signs are present. Dehydration can be treated by administering fluids orally or intravenously, depending on the severity.
If dehydration is left untreated, it can lead to a cascade of health issues, such as electrolyte imbalances, seizures, organ damage, and even death. Therefore, it’s crucial to seek medical attention immediately if symptoms of dehydration persist or worsen.
Biochemical Markers for Assessing Dehydration
Delving into the Realm of Laboratory Tests
When assessing the hydration status of an individual, healthcare providers delve into the world of biochemical markers. These markers, found within the serum, provide valuable insights into the delicate balance of fluids and electrolytes within the body.
Serum Sodium: A Key Indicator
Serum sodium is a crucial marker in gauging dehydration. Elevated levels, known as hypernatremia, signal dehydration, while low levels, or hyponatremia, indicate overhydration. Understanding these changes helps determine the severity and type of dehydration.
Potassium and Chloride: Electrolyte Balance
Potassium and chloride, two essential electrolytes, play a vital role in maintaining fluid balance within cells. Decreased levels can indicate dehydration, while elevated levels may suggest overhydration.
BUN and Creatinine: Measuring Kidney Function
Blood urea nitrogen (BUN) and creatinine are markers of renal function. Elevated levels of these markers may indicate dehydration due to inadequate kidney filtration.
Interpreting the Clues: Guiding Treatment
Interpreting the results of these biochemical markers helps healthcare providers make informed decisions about treatment and hydration levels. By assessing the severity of dehydration, they can determine the appropriate amount of fluids and electrolytes needed to restore balance.
The Importance of Prompt Action
It’s essential to address dehydration promptly, especially in vulnerable populations such as children and the elderly. Untreated dehydration can lead to serious complications, including organ failure. Biochemical markers provide critical information that aids in early detection and effective management of this potentially life-threatening condition.
Other Indicators of Dehydration
Beyond the typical clinical signs and biochemical markers, there are additional indicators that can provide clues about a patient’s hydration status.
One such indicator is the absence of dehydration or overhydration symptoms. A person who is well-hydrated will not exhibit signs like excessive thirst, dry mouth, decreased urination, or fatigue. Conversely, an overhydrated individual may experience symptoms such as swelling in the hands and feet, muscle cramps, or nausea.
Stable mental status is another important indicator. Dehydration can lead to confusion, disorientation, and irritability. However, a person with adequate hydration will typically have a clear and coherent mental state.
Tolerance of oral fluids is a valuable observation. A dehydrated person may have difficulty tolerating oral fluids, due to nausea or vomiting. In contrast, an adequately hydrated individual will be able to tolerate and absorb fluids without any issues.
Finally, the presence of no electrolyte imbalances is a positive sign. Dehydration can disrupt electrolyte balance, leading to problems like low sodium or potassium levels. However, in a well-hydrated person, electrolyte levels will be within normal ranges.
By considering these other indicators in conjunction with clinical signs and biochemical markers, healthcare professionals can make a more comprehensive assessment of a patient’s hydration status. This comprehensive approach helps ensure that individuals receive appropriate and timely treatment for dehydration or overhydration, promoting optimal health outcomes.
The Importance of Prompt Treatment for Dehydration
Dehydration can be a serious medical condition, especially for vulnerable populations like children and the elderly. It’s crucial to recognize and address dehydration promptly to prevent severe complications.
Dehydration Symptoms to Look Out For
Initial signs of dehydration can be subtle, so it’s essential to be vigilant. Dry mouth, rapid heartbeat, and sunken eyes are early warning signs. As dehydration worsens, symptoms intensify: fatigue, dizziness, muscle cramps, nausea, and decreased urine output.
Complications of Untreated Dehydration
Unattended dehydration can lead to serious health consequences. Severe dehydration can damage vital organs, cause electrolyte imbalances, and disrupt brain function. In extreme cases, untreated dehydration can result in seizures, cardiovascular arrest, or even death.
Seeking Medical Attention When Needed
If you experience persistent dehydration symptoms that don’t improve with home treatment, don’t hesitate to seek medical attention. Young children and frail elderly individuals should receive prompt medical evaluation even for mild dehydration.
Prompt Treatment Is Crucial
Early detection and treatment of dehydration are paramount. Fluids and electrolytes can be replenished intravenously in severe cases. For moderate dehydration, oral rehydration solutions (ORS) can effectively restore hydration.
Prevention: A Proactive Approach
Preventing dehydration is always better than treating it. Stay hydrated throughout the day, especially during hot weather or physical activity. Consume plenty of fluids, including water, sports drinks, or electrolyte-rich beverages. Fruits and vegetables also contribute to hydration and provide essential nutrients.
By understanding the signs, complications, and importance of prompt treatment for dehydration, we can take proactive measures to maintain optimal hydration and prevent its potentially debilitating effects.
Prevention Tips to Stay Hydrated: Stay Healthy, Stay Refreshed
Staying hydrated is crucial for our overall health and well-being. Dehydration, even mild, can lead to various unpleasant symptoms and even serious health consequences. By following these simple prevention tips, you can stay hydrated and safeguard your health:
Sip Water Throughout the Day
Make it a habit to sip on water regularly throughout the day, especially during hot weather or when engaging in strenuous activities like exercising or physical labor. Remember, thirst is often a sign that you’re already dehydrated, so it’s best to stay ahead of the curve and drink plenty of fluids.
Carry a Water Bottle
Carry a reusable water bottle with you wherever you go. This makes it convenient to have water on hand and encourages you to drink more frequently. Opt for bottles made from BPA-free materials to avoid potential health risks.
Enhance Your Water with Fruits and Vegetables
Add sliced fruits or vegetables to your water for a flavorful and hydrating twist. Not only does this boost the taste, but it also provides extra electrolytes and nutrients. Try adding slices of lemon, lime, cucumber, or berries to your water bottle.
Consume Electrolyte-Rich Foods
Fruits and vegetables are excellent sources of electrolytes, which are lost through sweat and need to be replenished. Incorporate electrolyte-rich foods into your diet, such as bananas, avocados, coconut water, spinach, or sports drinks when necessary.
Limit Sugary Drinks
While sugary drinks may provide temporary hydration, their high sugar content can dehydrate you in the long run. Instead, opt for low-sugar beverages like water, unsweetened tea, or flavored seltzer.
Monitor Your Hydration Status
Pay attention to your body’s signals and monitor your hydration status. Signs of dehydration include dark urine, fatigue, headaches, and **dizziness. If you experience these symptoms, increase your fluid intake and seek medical attention if they persist.